
Foreword
This year my annual report focuses on alcohol and specifically the harm caused by alcohol. It looks back through history examining our drinking habits of the past, the changing patterns of consumption and the harm it can cause to individuals, families and communities. It brings together the latest data, research, evidence and local insight to guide our shared efforts to do what we can to minimise the harm caused by alcohol.
The consumption of alcohol has been part of the diet and culture of many people in the UK for centuries. While many see the drinking of alcohol as a key social activity and it is very much normalised within our culture, alcohol consumption continues to be one of the leading causes of preventable ill health, disability, and premature death in the UK. Most notably the harm caused by alcohol is unequally felt with those already disadvantaged within society impacted most.
Alcohol shapes the health and wellbeing of our communities in profound ways; from the places we live and work to the opportunities we have to thrive. Reducing alcohol-related harm means more than changing individual behaviours. It requires us to build supportive environments together, strengthen social connections and ensure equitable access to care for everyone. In short reducing alcohol harm is everybody’s business.
The harmful impact of alcohol has been known for centuries. However, whilst successive governments have tried to limit the effects of harmful drinking, both alcohol consumption and alcohol related deaths have increased and alcohol consumption in the UK remains higher than the average when compared to Europe and countries such as Australia and America.
However, there is evidence that through the right evidence-based policies, programmes and legislation you can have a positive impact and reduce alcohol consumption. For example, when the Government introduced the duty escalator, which is the adjustment of duty rates each year in line with inflation, this saw alcohol-specific deaths level out when this was in place. However, in 2013 the Government reversed this policy, and we have seen alcohol-specific death rise. Scotland and Wales introduced Minimum Unit Pricing (MUP), which sets a minimum price of 50p per unit of alcohol sold, in 2018 and 2020 respectively. Alcohol-related deaths in Scotland fell by 13% with the greatest reduction in deaths seen in people living in the most deprived communities. England has not followed suit and in the absence of effective policy in England, the alcohol industry spends millions of pounds every year on targeted marketing campaigns portraying alcohol as a positive social activity.
Alcohol drinking patterns change over time. In the UK we are currently seeing consumption levels declining amongst younger adults but increasing in those over 55 years of age. In Devon rates of liver disease are rising rapidly, and we are currently seeing more deaths relating to alcohol than we have in decades.
It is important that we understand the increased risk of alcohol-related harm to those who drink alcohol. It is also important to recognise the harm it can cause to the wider family and communities across Devon. Increased alcohol consumption is associated with increases in domestic and sexual violence and abuse, anti-social behaviour and serious violence.
There is no doubt that alcohol plays a role in our society and that is unlikely to change but we need to understand the individual health risks and the wider societal harm caused by the current drinking patterns and levels in England and Devon. It is important that we focus on prevention to reduce the affordability and appeal of alcohol, intervene to help people early with potentially harmful drinking, and provide joined up care to those with more complex alcohol needs and dependency if we are to drive down consumption rates and reduce alcohol related illnesses and deaths in Devon.
By taking collective action through evidence-based policies, compassionate services and community partnerships, we can protect the health of our most vulnerable neighbours, empower individuals to make healthier choices and create a county where all residents can live well.
Steve Brown
Director of Public Health
1. Our drinking habits
Alcohol has been part of our diet and culture in the UK for centuries. The data on alcohol consumption in England over the past 200 years (Figure 1) is one of fluctuations, of peaks and troughs. The harm caused by alcohol consumption has been known about for a long time. The consumption of alcohol, specifically the drinking of gin increased in the middle of the 17th century, a period known as the ‘Gin Craze’ and depicted in Hogarth’s famous ‘Gin Lane’ picture which represented widespread drunkenness and saw an increase in crime and poverty. This period saw the introduction of the (Sales of Spirits Act 1750), commonly known as the Gin Act 1751.
Figure 1: Estimated per capita consumption 1800-1935
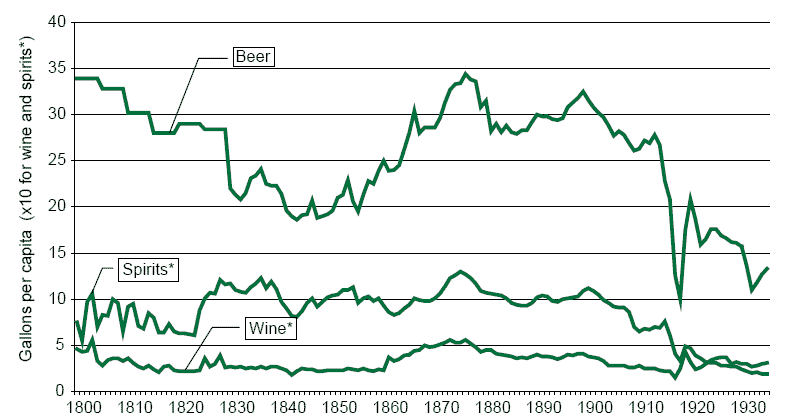
Source: G. Wilson, Alcohol and the Nation
While drinking habits in England did fluctuate there was an overall long-term downward trend which lasted until the mid-20th century before there was a significant increase in consumption. More recent data shows that alcohol consumption has fallen in the UK since the start of the century but is now rapidly increasing again since the COVID-19 pandemic.
Figure 2: Average number of units of alcohol drunk per week by adults aged 16 and over in England, 2011-22
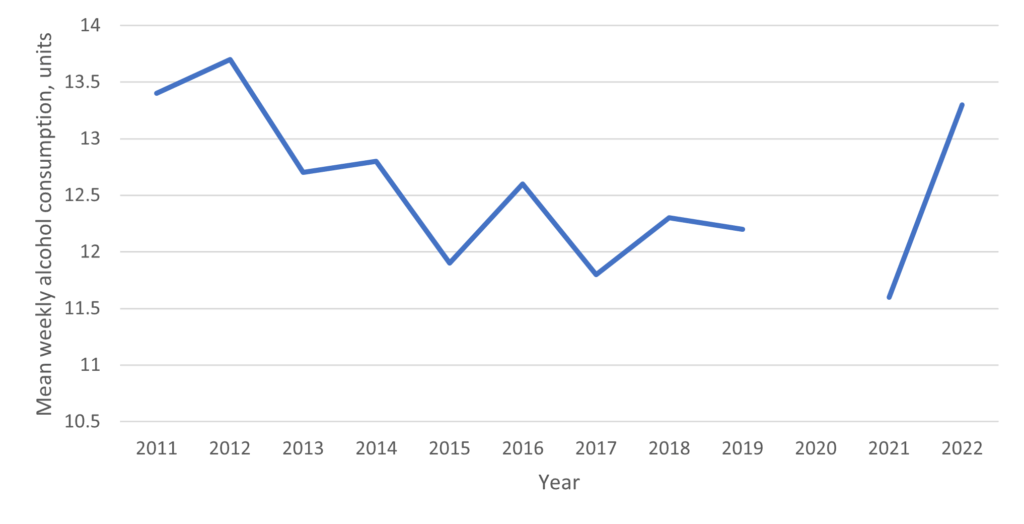
Source: G. NHS Health Survey for England, 2022. Note: no data was collected in 2020.
Changing Patterns of Alcohol Use
While we see a change in overall drinking habits, we also see a change in drinking habits amongst specific age groups and genders.
Age-Related Trends
Nationally, alcohol consumption is declining among younger adults (18–34), driven by factors such as cost, health awareness, alternative substances, and changing social habits. This shift has increased demand for low and no-alcohol drinks, especially among younger and more affluent groups. If this continues and without broader policy changes, this trend could see a widening of health inequalities. Nationally we are seeing alcohol use increase amongst older adults (55+ years).
In the Southwest, the picture is mixed, with harm increasing in some groups and decreasing in others. The data shows that fewer people drink during early pregnancy, and more adults are abstaining altogether. However, high-risk drinking is rising, while lower-risk drinking is declining.
Many have continued heavy drinking patterns established during the COVID-19 pandemic, contributing to a record 10,473 alcohol-specific deaths in England in 2023.
In Devon, alcohol continues to cause significant harm among under-18s. Despite national declines, Devon’s admission rates for alcohol-specific conditions in this age group remain nearly double the national average and have been consistently high since 2012.
Gender differences
While men have historically consumed more alcohol, the gender gap is narrowing. Among younger adults, women now drink at similar or higher levels than men. In Devon, under-18 girls are more than twice as likely as boys to be admitted for alcohol-specific conditions. However, men are still twice as likely to die from alcohol-related causes as women.
2. Alcohol harms

- Alcohol is a leading cause of preventable ill health and deaths in the UK
- Alcohol can lead to immediate and long-term impacts on health and wellbeing, with harms impacting on society
- Alcohol related harm is more pronounced in communities facing higher levels of deprivation
Alcohol consumption continues to be one of the leading causes of preventable ill health, disability, and premature death in the UK. Its impacts are wide-ranging, affecting individuals, families, and communities across Devon. While often perceived as a normal part of social life, alcohol use carries significant risks that can emerge both immediately and over the longer term.
Figure 3: Health impacts of harmful use of alcohol
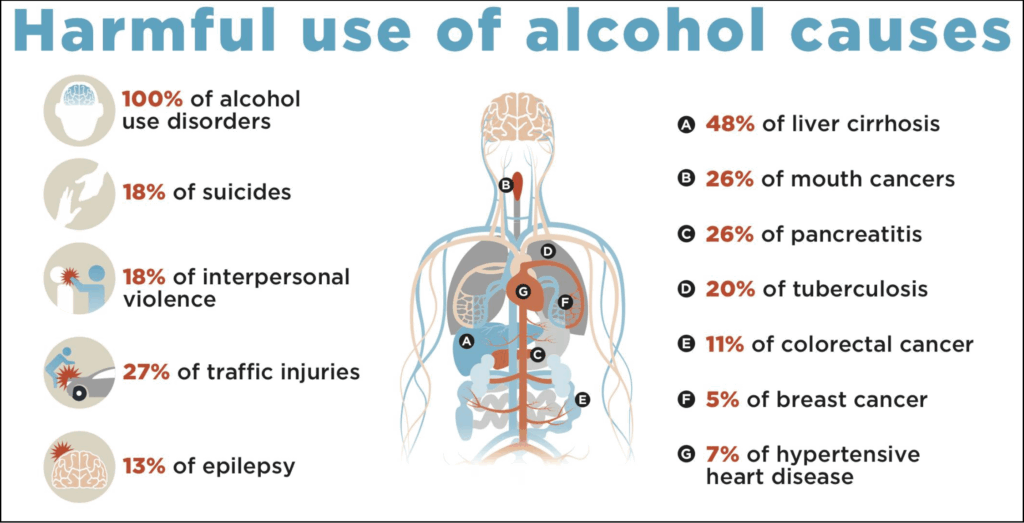
Source: World Health Organisation 2025
Understanding risk levels
Until recently it was believed that drinking a small amount of alcohol might actually be good for your health. Science has now demonstrated that this is not the case and that no level of alcohol is completely safe. However, risks increase with higher consumption. Drinking is typically classed as:
- No risk: Not drinking at all
- Lower risk: Up to 14 units per week
- Increasing risk: 15–35 units (women), 15–50 units (men)
- Higher risk: Over 35 units (women), over 50 units (men)
- Binge drinking: Over 6 units (women) or 8 units (men) in one sitting
A unit of alcohol if 10 millilitres of pure alcohol. The following figure show the number of units typically contained in various alcohol drinks.
Figure 4: Units of alcohol contained in different alcohol drinks

Source: Adapted from Alcohol Concern
Alcohol Change UK have a unit calculator that can be used to find out how many units are in a particular drink, or to check how much you’re drinking. Further advice and support for reducing the amount of alcohol you drink is available here: Alcohol advice – NHS.
Short-Term Harms
The consumption of alcohol has some short-term impacts. We know that alcohol impairs judgement, coordination, and reaction times, increasing the risk of accidents, injuries, and risky behaviours such as drink-driving or unsafe sex. It’s a major factor in emergency hospital attendances and can cause alcohol poisoning, which can be life-threatening. Alcohol-related harm can also affect others through violence or antisocial behaviour. When alcohol is mixed with other substances, legal and illicit, the risk of harm multiplies through, for example unpredictable interactions, increased risk of overdose and severely impaired function.
Long-Term Harms
Regular drinking raises the risk of serious health conditions including heart disease, liver disease, stroke, and several cancers. Alcohol is a known carcinogen, directly causing around 3.3% of UK cancer cases. It also affects mental health, increasing the risk of depression, anxiety, and alcohol-related brain injury, which can lead to cognitive decline and dementia.
Dependence and Hidden Harm
High-risk drinking can lead to dependence, where suddenly stopping alcohol can be dangerous without medical support. However, even those who are not dependent can suffer harm. Binge drinking, often underestimated, can cause liver damage, and many people may be harming their health without realising it.
Local Impact in Devon
Devon’s alcohol services are seeing more and more people with established liver disease, often after years of heavy drinking. While reducing or stopping alcohol can slow disease progression, early intervention is crucial to prevent irreversible harm.
The data for alcohol harm show a significant and growing burden of alcohol-related harm in Devon.
Data for Devon indicates:
- Alcohol-specific mortality has risen by 18.5% since 2006, reaching 10.93 deaths per 100,000 in 2023
- Under-75 mortality from alcoholic liver disease has increased by 41.9% since 2001
- Alcohol-related hospital admissions have grown by 46% since 2016/17
- Admissions for alcoholic liver disease have surged by 70% over the same period.
Figure 5: Drinking patterns in the South West
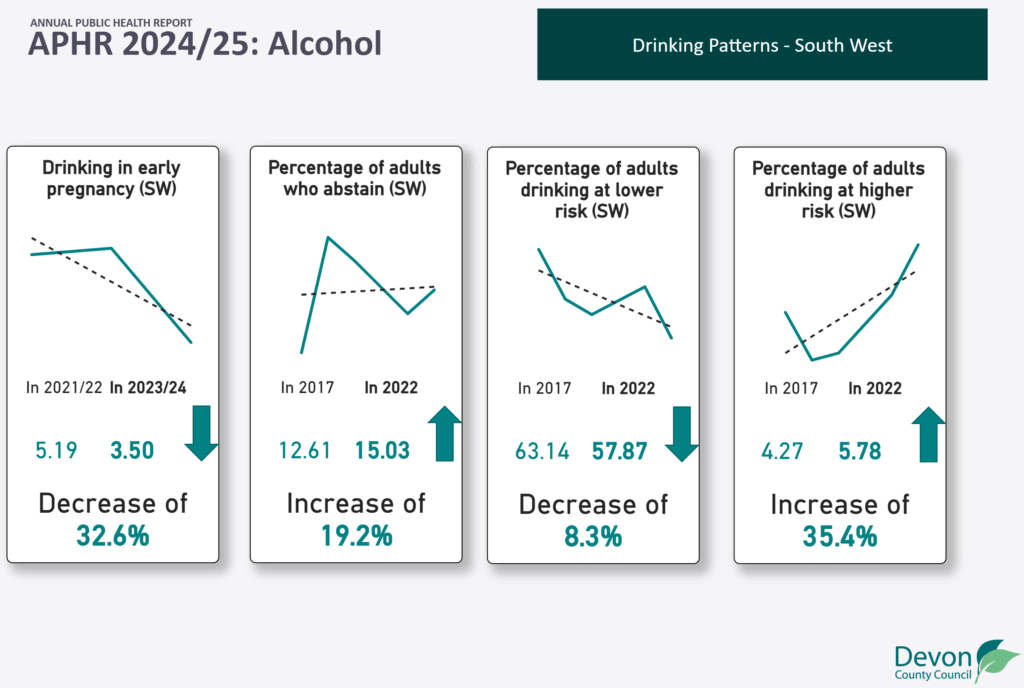
Source: Devon Annual Public Health Report 2024/25 Alcohol Dashboard
Figure 6: Short-term impacts of alcohol in Devon
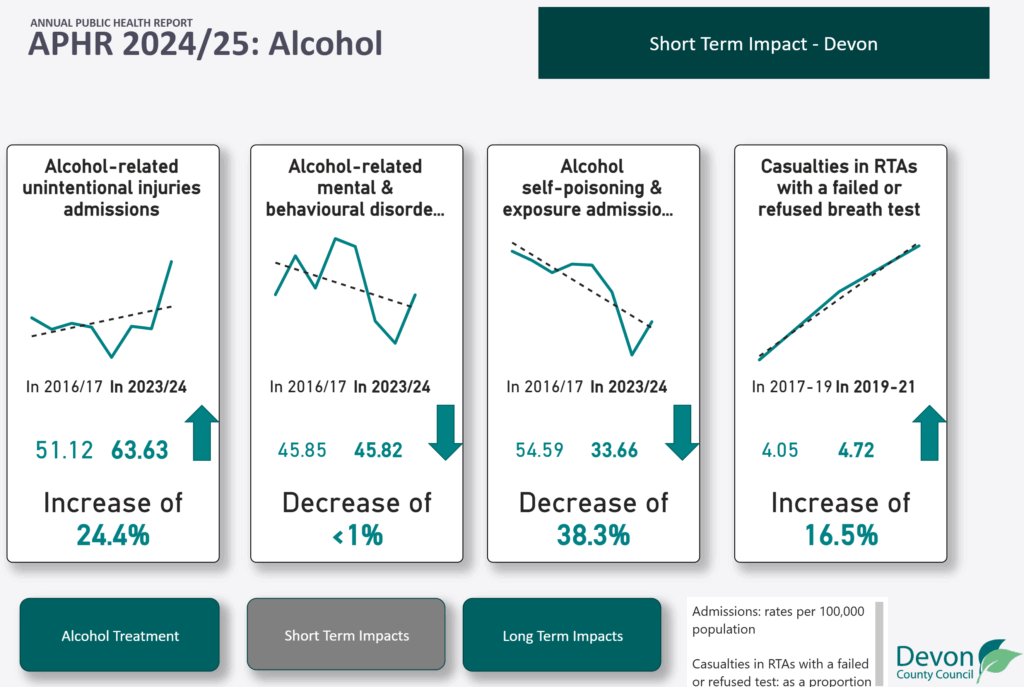
Source: Devon Annual Public Health Report 2024/25 Alcohol Dashboard
Recent data for Devon highlights a mixed picture of short-term alcohol-related harm:
- Alcohol poisoning and exposure admissions have decreased by 38.3% since 2016/17, indicating some progress in reducing the most acute forms of harm.
- In contrast, alcohol-related unintentional injury admissions have risen by 24.4%, with a notable increase in the last two years, suggesting growing risks linked to impaired judgement and accidents.
- The proportion of road traffic accident casualties involving a failed or refused breathalyser test has increased by 16.5% since 2017, pointing to ongoing concerns around drink-driving.
- Admissions for alcohol-related mental and behavioural disorders have remained largely unchanged.
Figure 7: Long-term impacts of alcohol in Devon
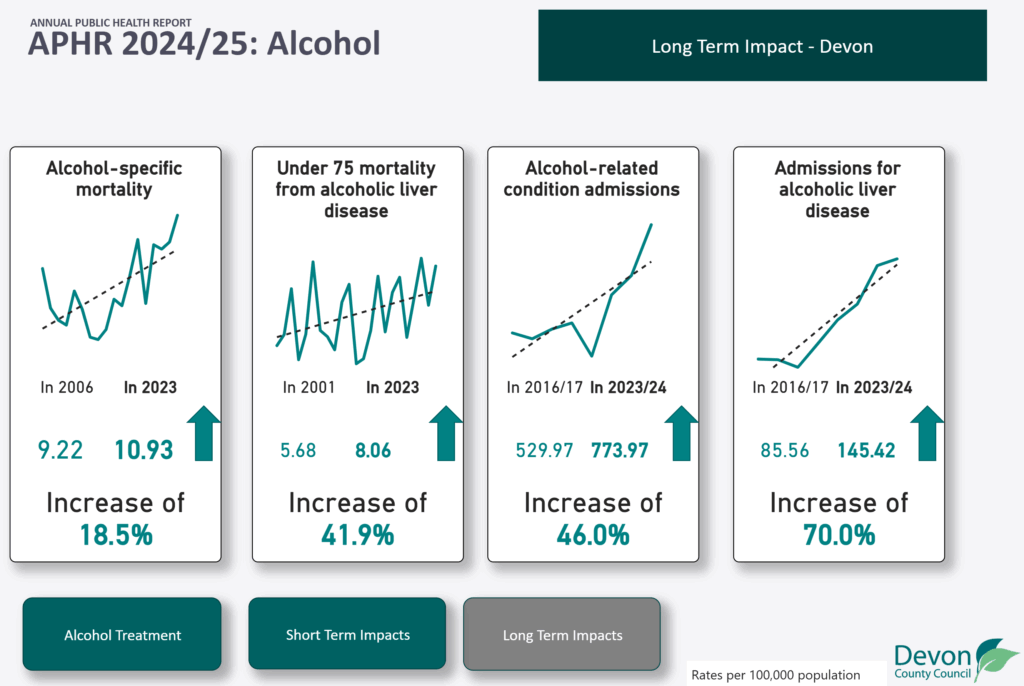
Source: Devon Annual Public Health Report 2024/25 Alcohol Dashboard
- Alcohol-specific mortality has increased by 18.5% between 2006 and 2023, while a reduction in the mortality rate was initially observed, recent years show a sharper increase.
- Although fluctuating, the overall trend for the Under 75 mortality rate from alcoholic liver disease has risen by 41.9% between 2001 and 2023.
- Alcohol-related condition admissions have increased overall by 46.0% between 2016/17 and 2023/24, alongside admissions for alcoholic liver disease increasing by 70.0% over the same period.
- The above suggests that the longer-term impacts of alcohol across Devon are worsening.
Treatment
Not everyone with high alcohol use needs specialist treatment. Many benefit from brief advice, lifestyle support, community groups, or digital tools tailored to their needs and preferences.
Public Health Devon commissions ‘Together’ a Drug and Alcohol Service to support adults living in Devon experiencing harm from alcohol or drug use, whether that harm affects their health, relationships, housing, employment, or finances.
Figure 8: Alcohol treatment in Devon
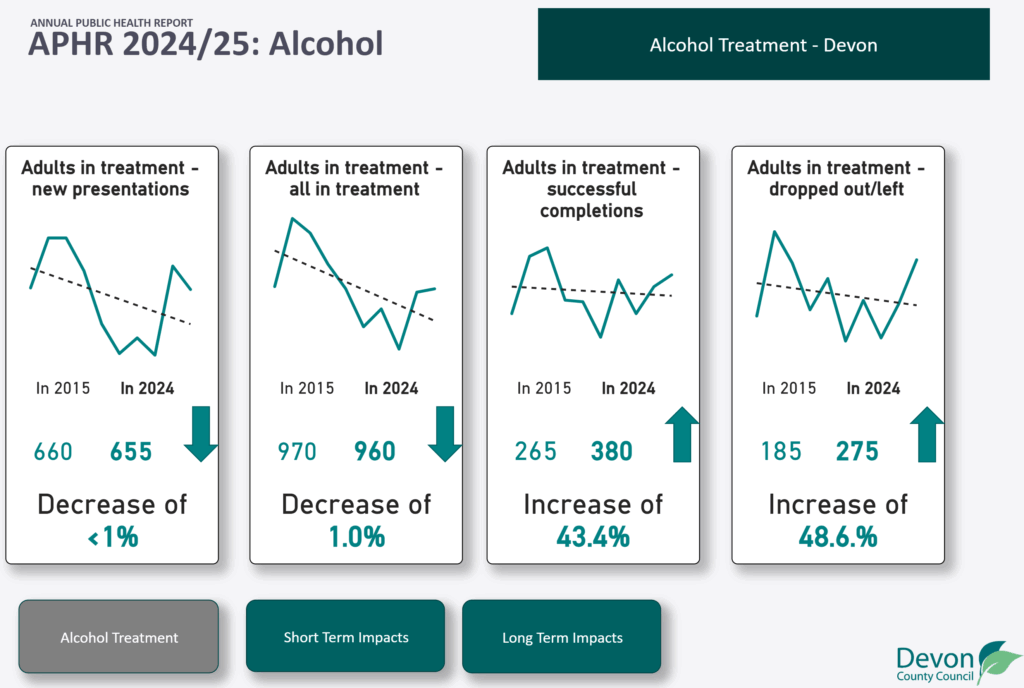
Source: Devon Annual Public Health Report 2024/25 Alcohol Dashboard
In 2024, 960 adults were in specialist alcohol treatment in Devon, this marks a recent increase in numbers in treatment and a near return to 2015 levels. Public Health Devon has been in receipt of additional funding to help implement the national drugs strategy and it is the use of this additional funding which has helped with more treatment capacity. This is against a backdrop of a reduction in the Public Health Grant over the past decade.
Among those exiting treatment in 2023-24, 54% successfully completed their treatment, on par with national averages of 55%. However, recent local data suggests this proportion may be dropping. This may be due to the national push in the last 3 years to increase numbers in treatment, which increases recovery worker caseloads, meaning treatment quality may suffer.
For more data and information, please visit: Alcohol Dashboard – Devon Annual Public Health Report 2024/25 – Devon Health and Wellbeing
Wider societal harms
The long-term impact of alcohol extends beyond health, affecting relationships, employment, and financial stability. The social consequences of alcohol use ripple through families and communities. It is a key factor in domestic violence, child neglect, and crime. Local health and social care services also experience alcohol-related pressures, with alcohol contributing to increased demand on emergency departments, ambulance services, mental health provision, and social services.
It is estimated that the total societal cost of alcohol harm in England in 2021-22 was £27.4 billion, equivalent to 1.2% GDP. The total cost per year alcohol costs £316m per year in Devon , which is £388 for each person living in Devon. This is over 10 times the size of the Public Health Grant for Devon which is used to deliver prevention activity alongside crucial services such as drug and alcohol treatment, sexual health services and health visiting. Most of this cost is due to crime and disorder, followed by costs to the NHS, the wider economy due to lost productivity, and social care.
These increasing consumption trends and the significant and growing burden of alcohol-related harm in Devon, reinforcing the need for prevention strategies, early intervention and support and treatment access to reduce immediate alcohol-related risks.
3. National Alcohol Policy Context (England)

The importance of having a clear national strategy to tackle alcohol harm is essential. The Government launched an alcohol strategy in 2012 which contained a commitment to introduce a minimum unit pricing on alcohol to drive down alcohol consumption levels. However, following a public consultation it was never introduced in England, unlike in Scotland and Wales. More recently, the 2021 national drugs strategy committed to expanding support for alcohol and drug treatment, with a target of 54,500 new treatment places across England by 2024/25. Additional local funding has been allocated by central Government to support delivery of the new strategy but unfortunately funding is only confirmed on an annual basis making it difficult to plan for new treatment places over a longer period.
The Government launched its new 10-year health plan for the NHS in July 2025 ( Fit for the future: 10 Year Health Plan for England). The plan highlights the impact of alcohol has on individuals and the wider society and to help tackle this has committed to by introducing a mandatory requirement for alcoholic drinks to display consistent nutritional information and health warning message. In addition, the government recognises the importance of enhancing public awareness of the health risks of alcohol consumption and to help people make more informed healthier choices they will be introducing a mandatory requirement to bring alcohol labelling in line with existing health and nutritional labelling requirements for tobacco, food and alcohol-free drinks.
The 10-year plan also make a commitment to work with local government to roll-out of effective community led schemes which evidence reductions in alcohol harm such as peer-led support groups, peer mentoring and coaching and mutual aid networks.
Impact in Devon
Devon’s alcohol services are seeing more people with established liver disease, often after years of heavy drinking. While reducing or stopping alcohol can slow disease progression, early intervention is crucial to prevent irreversible harm.
NHS Healthcare initiatives: The NHS Long Term Plan supports Alcohol Care Teams in hospitals with high alcohol-related admissions. These teams are jointly funded by NHS and Local Authorities with this intervention showing positive outcomes in emergency presentations and admissions across pilot areas nationally. NHS funding has not yet enabled these to become fully established in Devon.
Criminal Justice initiatives: Several national initiatives have been introduced to address alcohol-related offending. Since 2021, courts can impose Alcohol Abstinence Orders with sobriety tags. These reduce reoffending when paired with treatment. “Problem-solving courts” and alcohol treatment requirements are also being trialled, though most harmful drinkers are not in contact with the criminal justice system.
Prevention: The Government has announced that it wishes to increase its focus on prevention with one of its 3 core missions for the NHS to move from ‘Treatment to Prevention’. The alcohol duty was raised in February 2025 and updated clinical guidelines are expected and there is hope for a new national alcohol strategy, focusing on population-level approaches and clearer local responsibilities. If a national strategy is to be produced, it will need to contain clear policy decisions on advertising and promotion of alcohol.
Local Policy Context (Devon)
In response to the publication of the national Drugs Strategy in 2022, Devon County Council and partners formed the Devon Drug and Alcohol Strategic Partnership (DDASP). This meeting is chaired by me as the Director of Public Health. The partnership focusses on delivering the national drug strategy goals and local priorities, improving treatment and recovery and reducing drug and alcohol-related deaths. There is a separate group which looks specifically at reducing alcohol related harm.
Devon must utilise their ring-fenced public health grant to fund specialist drug and alcohol treatment services for Devon residents. Devon County Council receives a sum of £39.29 per head to fund all public health services within Devon. The allocation places Devon County Council in the bottom 10 local authorities in the country in terms of public health grant allocation as the DHSC use a deprivation-based funding formula to allocation funding. Since the publication of the Drugs Strategy all local authorities have also received an additional ring-fenced funding for alcohol and drug treatment to support the delivery of the national strategy. This funding is only confirmed on an annual basis making it difficult to make longer term decisions on treatment services.
All local authorities and the NHS have a duty to tackle health inequalities, and we know that alcohol must be a key focus if we are to reduce health inequalities in Devon. It was included in the 2023–24 Annual Public Health Report, Health in an Ageing Devon and it is highlighted in the Joint Strategic Needs Assessment and NHS Devon ICS Strategy The Devon Roadmap.
In addition to individual harm caused by harmful drinking we also know that alcohol impacts on the wider community. Local authorities use existing powers to address alcohol-related harm and work with the police, trading standards and wider partners, including businesses, to implement and enforce licensing policies and requirements under the Licensing Act 2003. The Police and Crime Commissioner’s 2025–29 plan prioritises drug and alcohol issues, including support for visible policing in the night-time economy.
Increasing work on prevention is vital. Alcohol education is embedded in the statutory PSHE (personal, social, health and economic) curriculum in schools. The Devon Schools Wellbeing Partnership supports schools with guidance and resources. Y-SMART, Devon’s young people’s drug and alcohol service, provides targeted education and support, including one-to-one and small group sessions.
4. What shapes our relationship with alcohol: the determinants of alcohol harm
Alcohol use and its harms are shaped by a complex combination of personal, social, economic, and environmental influences. There is growing recognition that the conditions in which people live significantly affect both drinking behaviours and the risk of harm.
There are two key types of vulnerability which influence how alcohol impacts health and wellbeing. These include:
Societal vulnerability factors: Alcohol pricing, availability, affordability, advertising, regulation, drinking context, social economic status, major incidents and culture.
Individual vulnerability factors: Mental health, experiences of trauma, homelessness, neurodiversity, age and genetics.
These factors can interact with one another, compounding risks. Understanding the broader factors behind alcohol-related harm shifts the focus from individual choices to collective responsibility. Reducing harm in Devon will require not just supporting healthier behaviours, but also shaping environments that make those choices easier, safer, and fairer.
Figure 9: Determinants of alcohol harm
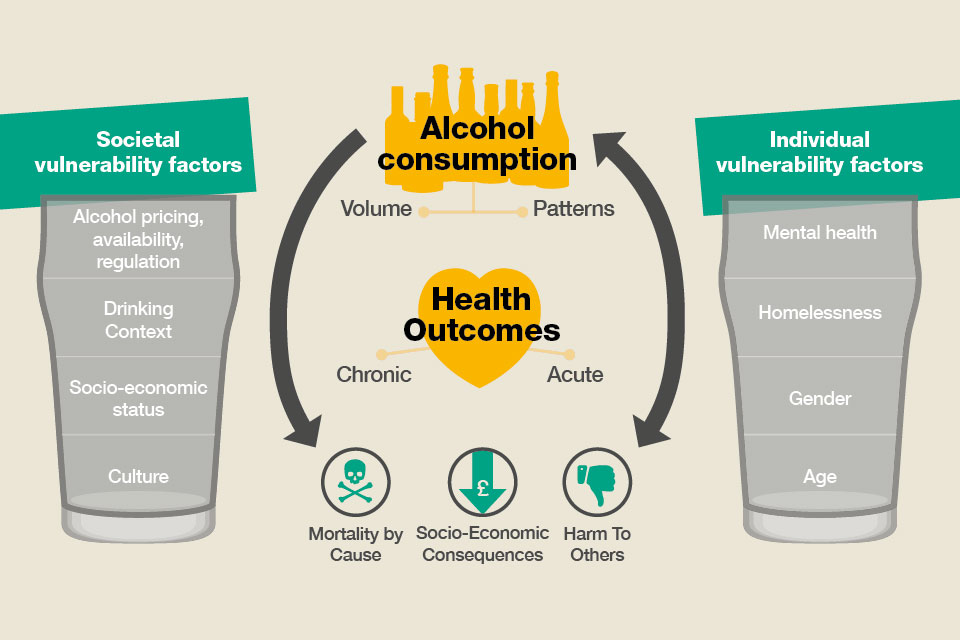
Source: Adapted from Health matters: harmful drinking and alcohol dependence – GOV.UK
For more detailed information on society and individual vulnerability factors please visit our supporting report: The Detail Behind the Story
5. How do we reduce alcohol harm in Devon

Reducing alcohol harms in Devon will require the whole system including local authorities, primary care, acute services, specialist treatment services, the voluntary and community sector and social care to work together to tackle this shared challenge.
Figure 10 outlines prevention activity to reduce alcohol harm, action ranges from addressing the wider determinants of alcohol use through to treatment services.
Figure 10: Defining prevention for alcohol usage
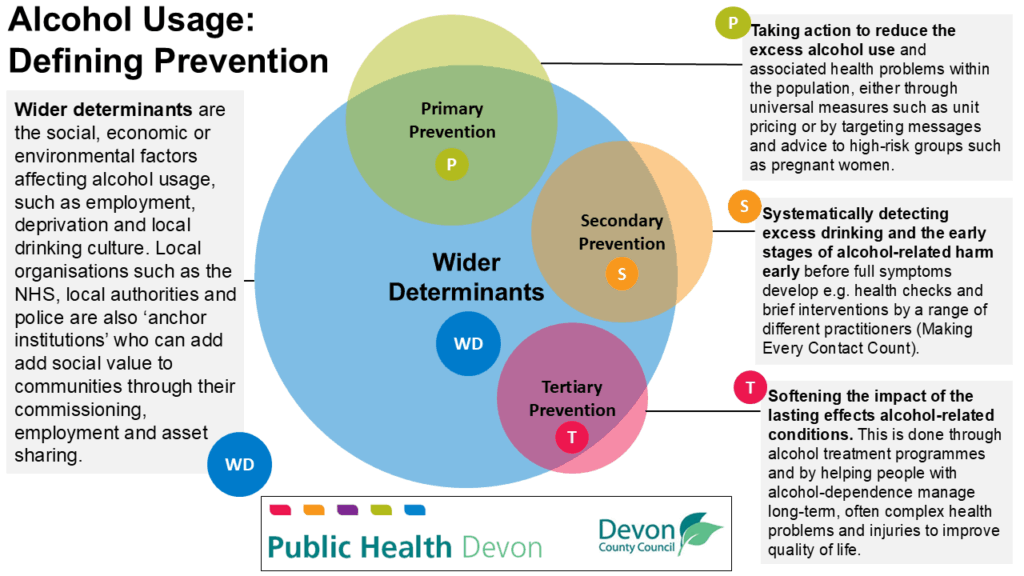
Source: Devon County Council Public Health Team, 2025
Wider determinants
Devon County Council and the wider local system in Devon have a role in shaping the wider determinants of health to reduce alcohol harms by addressing the social, economic and environmental conditions that shape drinking behaviours and vulnerability. Local authorities and their partners can influence these wider determinants through regulation of the physical environment, civic leadership, commissioning of services and strategic partnerships. By embedding health equity in planning, housing, education, employment and community safety, Devon can create conditions that both reduce demand for alcohol as a coping mechanism and strengthen protective factors against harm.
Primary prevention: Population-based approaches
Primary prevention approaches impact the most people and can shift the whole dial on alcohol use in the population, for example:
- Minimum unit pricing
- The alcohol duty escalator
- The wider impact of the Licensing Act and Public Health influence on policies
Advertising restrictions target another key driver of drinking norms. This is challenging without national policy or legislation but local action on responsible advertising can start to change the narrative.
Secondary prevention: Early Intervention
Secondary prevention; identifying risk drinking early and offering advice, is a notable gap in the current Devon system. NHS Health Check numbers are increasing and Making Every Contact Count (MECC) training has been provided but there is not a systematic and system wide approach in Devon.
Brief advice through Make Every Contact Count, NHS Health Checks and the adoption of the Audit C tool. Early identification and brief intervention in both healthcare and community settings are proven approaches to reducing hazardous drinking. In primary care, emergency departments and antenatal services, the use of validated screening tools such as AUDIT-C followed by brief advice has been shown to reduce alcohol consumption by an average of two to three units per week. The NHS Health Check includes an alcohol risk assessment. Availability depends on local GP or pharmacy capacity but numbers are increasing and a more targeted approach has been implemented.
Longer structured behaviour change approaches. More intensive behaviour change techniques can lead to greater decreases in alcohol consumption for those looking to cut down on their drinking. These can be app-based, face-to-face or remote over video call or telephone. Larger improvements in alcohol consumption seem to be related to having some personal contact with a practitioner, comparing alcohol consumption to average population levels, feedback on performance and commitment to personal goals. Simply providing information on alcohol harms produces smaller results.
Tertiary prevention: Supporting People with Alcohol Treatment Need
People who need treatment for alcohol dependence come from all parts of Devon and from all walks of life. While this group represents a smaller proportion of those affected by alcohol overall, the level of need is often more complex and the impact on individuals and their families can be profound. Recovery is not a one-size-fits-all process: it requires personalised support that recognises the full picture of someone’s life. Evidence shows that the best outcomes come from services that help people build their recovery capital: stable housing, supportive relationships, access to healthcare, and opportunities to reconnect with their communities.
Tertiary prevention supports those with harmful or dependent alcohol use through:
- Specialist treatment services for adults and young people, including in-patient and community detox services
- Joined up care between treatment services, primary care and acute services for relapse prevention and support for the health outcomes of long-term alcohol use
- Community groups and activities which build meaning and recovery capital to support recovery.
Joined up services. The evidence highlights that action to reduce alcohol harm is far more than just a treatment service issue. People dependent on alcohol often have complex interlocking needs and can easily fall through the cracks in services if they are not joined up. This includes a range of interlinking services.
- Mental Health and Substance misuse
- Joined up acute care
- Integration with employment and housing
- Relapse prevention in primary care
- Alcohol related brain injury pathways
Systems that link beyond healthcare services such as housing and employment can be life changing for people struggling with alcohol.
For more detailed information on what works in practice please visit our supporting report: The Detail Behind the Story
Reflections
The report is clear that alcohol harm is increasingly impacting on individuals, families and Devon communities. While some of the known evidenced-based interventions require a commitment and decision by central government we know that there are things we can do locally to reduce alcohol harm. We, as the Devon health and social care system could provide support those experiencing alcohol dependence, and these need to be addressed. However, prevention is always better than cure. Efforts to reduce the availability, affordability and normalisation of alcohol, support to reduce vulnerability towards addiction, and early identification and help will prevent many people from ever needing treatment services. Even more impactfully, it will prevent the multitude of more common harms to society and to individuals and families that come about due to even non-dependent alcohol use.
Alcohol harm in Devon is everybody’s business. It is a whole-system problem which must have a whole-system answer. We urge everyone to play their part in tackling the growing issue of alcohol harm in Devon.
6. Recommendations
- Work with partners, communities and individuals to increase the awareness and understanding of alcohol harm.
- Develop a shared Devon alcohol strategy informed by evidence and data, local intelligence and the voice of lived experience to build collective understanding and shared responsibility for reducing alcohol harm.
- Work in partnership to optimise all age pathways for primary, secondary and tertiary prevention, building capacity and capability within the system and addressing gaps for those with an alcohol need with a focus on joined up services and increasing investment where possible.
- Continue to address the wider determinants of health including employment, housing and community safety, including work with partners to ensure the availability of safe housing for those with alcohol dependency according to housing-first principles.
- Embed identification and brief advice in public-facing roles across the statutory and VCSE sectors in Devon, especially where people may be most vulnerable to alcohol harms.
- Explore how to improve access to alcohol treatment for those who need it most through reviewing and improving the referral and self-referral processes and supporting GPs and other professionals in understanding and using these processes.
- Work in partnership with Devon local authorities to standardise and share alcohol licensed premises data alongside health, communities and crime data to better understand where licensing decisions may have a beneficial impact on health and wellbeing and to limit the growth of licensed premises in problem areas alongside continuing to advocate for a Public Health Licensing objective for decision making.
- Ensure sustainable support for community hubs that support people struggling with alcohol harms and, more broadly, disadvantage.
- Through the Association of Directors of Public Health continue to lobby Central Government for the reintroduction of the tax escalator on alcohol and the introduction of Minimum Unit Pricing in England.
7. Joint Strategic Needs Assessment (JSNA)

The Joint Strategic Needs Assessment (JSNA) looks at the current and future health and care needs of the local population and it is a legal requirement of the Health and Wellbeing Board to produce and publish a JSNA. The assessment informs and guides the planning, commissioning and delivery of local health, wellbeing and care services. For more detailed JSNA information, data and intelligence, please visit Joint Strategic Needs Assessment – Devon Health and Wellbeing.
Devon is the third largest county in the country with beautiful natural environment and history attracting many residents and tourists to live and visit the area. Devon has great potential in providing individuals and families with the opportunity to live a healthy and fulfilled life. Like many areas, there are challenges which exist for Devon residents which can impact upon this ability to live a healthy life.
8. Recommendations 2023-24 Update
| Recommendations 2023-24 | Update on Progress |
| Establish a workstream focused on developing predictive analytics to inform service planning across Public Health, Adult Social Care, Health and wider local authority services. | A workstream was established in 2024-25 focused on predicting future demand for Public Health, Adult Social Care and Health services in Devon. This workstream established overarching principles and methodologies that have been applied in planning, market position statement and Joint Strategic Needs Assessment work. Further to this a Data and Intelligence Board was established for Devon County Council in 2024-25 to implement the recommendations of an organisational data and intelligence review. This review included a review of advanced analytical skills, including predictive analytics, and made a specific recommendation to develop a learning set approach to boost organisational skills in particular areas, including predictive analytics. |
| Develop a dementia strategy to ensure there is an agreed and clear strategy for Devon. | A system wide Dementia Strategy has been developed and produced by the Devon Dementia and Memory Care Oversight Group it has been presented at a number of forums and is awaiting publication |
| Increase targeted action on promoting people staying active physically, mentally and socially. | A range of programmes and activities across partners and within communities continue to support individuals throughout adulthood including Active Devon who run a number of targeted initiatives. Naturally Healthy through the Local Nature Partnership combines activity with wellbeing support in the natural environment. Five Ways to Wellbeing continues to raise awareness on how to stay well. |
| Explore the adoption of Devon as a World Health Organization Age friendly community. | Public Health Devon continues to work with partners to make Devon a WHO Age Friendly Community, a report was submitted to the Devon Health and Wellbeing Board to seek commitment to develop a local approach Healthy Age Friendly Communities.pdf |
| Deliver on the Smoke-free generation ambitions and scale up our offer to support more smokers to quit. | The Smokefree Generation programme has been designed as part of a collaborative system, using behavioural science and taking a proportionate universalism approach to offer a range of support options for those in Devon looking to quit smoking. To advance our ambitions, we have strengthened and expanded the Smokefree Generation Team within Public Health, enhancing our leadership, commissioning, and delivery capabilities. In collaboration with the voluntary, community, and social enterprise (VCSE) sector, we funded ten targeted projects to support smoking cessation efforts in priority groups. To further broaden our reach, we commissioned the Smoke Free App, alongside tailored advertising campaigns aimed at key demographics. We have expanded our specialist stop smoking service, Stop for Life Devon, which continues to exceed expectations, with increased referrals and a high quit rate of 71%. We are working closely with local hospital trusts to strengthen tobacco dependence pathways, funding resources and exploring dedicated roles to support community patients. Primary care continues to receive funding for tobacco dependence services, with increased support for service delivery. Overall, we have supported 2511 people to set a quit date during 2024, largely from groups disproportionately affected by the harms of tobacco; a number which is steadily increasing with further investment in Devon. |
| Work with key partners to increase action on the early identification and intervention of key health conditions, including high blood pressure, type 2 diabetes, dementia, people at risk of falls. | Significant work has been undertaken on CVD Prevention, which includes action to prevent and treat hypertension, prevent type 2 diabetes and delivery of NHS health checks which in addition to identifying CVD risks, also raises people’s awareness of early symptoms of dementia and informs them where to get help. One Devon CVD Prevention Partnership Devon Public Health chairs the CVD Prevention Partnership which plans co-ordinated activity across Plymouth, Devon and Torbay. The partnership have a refreshed and resourced action plan for 2025-26 and CVD Prevention has been agreed as a System priority. The partnership were successful in its bid to become one of 6 areas nationally to benefit from the CLEAR Healthy Living 3 Programme, which improves approaches to CVD Prevention in GP practices, particularly focusing on hypertension. NHS Health Checks Devon’s delivery of NHS Health Checks through GP Practices is steadily increasing and a higher proportion of those offered have received a check. A total of 19,981 Health Checks were delivered across Devon over 24/25. Going forward, a new specification will support GP Practices to target a greater proportion of checks to communities and individuals most likely to benefit. A targeted outreach service has been commissioned and is being delivered by the Royal Devon United Health Care Trust Outreach Vaccination Team. They are focusing delivery in rural and coastal locations and on groups who are under-served by the main offer, such as those in routine and manual occupations. The team have completed 1036 targeted Health Checks this year, with excellent feedback. Hypertension case finding A One Devon approach to hypertension case finding and “Know Your Numbers” campaigns have been developed. A coordinated Devon-wide campaign is being planned for September 2025. We have worked with Libraries Unlimited to develop a Devon-wide BP Machine Loan Scheme across all 50 libraries. The launch will coincide with Know Your Numbers week. Hypertension has been the focus over the past year and recent CVD Prevent data demonstrates that as a partnership we are making an impact. Falls Prevention Devon ICB convened a Devon-wide event in December 2024 to draw together the wide ranging work on falls and frailty across the county. A co-ordinating structure with a development group has been proposed, chaired by Dr Kay Brennan, working through Local Healthy Ageing Boards. The focus will be on Digital technology for falls preventionPrevention of falls in care homes Improved data and information Physical Activity for Older People Training and awareness Early diagnosis and proactive care |
| Support the national epidemiological survey on oral health in people aged 65yrs+ in care homes. | The local Community Dental Services were unable to complete the national epidemiology survey on oral health in people aged 65yrs+ in care homes due to competing priorities as they had to focus their limited clinical dental capacity on reducing waiting lists for Devon residents. Public Health Devon is working with NHS Devon to ensure there is a sustainable long-term solution that will enable Devon to participate in future surveys which are crucial to understanding how to improve oral health and dental care in Devon. |
| Maintaining high attendance at national screening and uptake of national immunisation programmes | Screening uptake in Devon in 2023/24 or 2024 is above the national average for breast cancer, bowel cancer, abdominal aortic aneurysm (AAA), and cervical screening. The uptake rate has increased for bowel cancer, AAA screening and remained stable for breast and cervical cancer screening in those aged over 50. In 2023/24 shingles vaccination uptake is similar to nationally, the pneumococcal polysaccharide vaccine (PPV) uptake in Devon for people aged over 65 is in line with the national average but uptake is showing an increasing annual uptake trend. Uptake of Flu vaccinations in over 65s is above the national average, and although not a significant change, the uptake rate is showing slight decline each year so the ensuring strong messaging around the importance of annual vaccine uptake is still a priority locally and nationally. |
| Equality impact assessments should be undertaken on all policy decisions to ensure that proposed actions are proportionately targeted at the most deprived communities to tackle health inequalities. | Equality impact assessments continue to be undertaken for significant policy and programme decisions to ensure there is an impact on health inequalities. See published assessments: Published Impact Assessments – Impact Assessment |