Annual Public Health Report 2021-22
1. Introduction
This is my second Annual Public Health Report for Devon County Council. My report last year, not unsurprisingly, focused on COVID-19, highlighting the impact the pandemic had on individuals, families and communities within Devon and how agencies and community groups came together to respond to the pandemic and support one another. While we all may have hoped that COVID-19 would not have needed to be included within this year’s annual report this unfortunately is not the case. My report this year does continue with the story of the Pandemic and examines the wider impact and what ‘living with covid’ looks like.
The evidence is clear, and I included a chapter in my report last year, that the COVID-19 pandemic has impacted disproportionality on certain groups amongst the population and many people in these groups were suffering poor health before the pandemic, so the pandemic has made the health of these individuals worse.
My report also examines the current ‘cost-of-living crisis’, being driven by rising energy, fuel and food prices, and inflation currently at its highest rate for 30 years. The ‘cost-of-living crisis’, is clearly having an impact on all Devon residents but as with the pandemic we know the impact with be felt most by those in greatest need. The report highlights the potential impact on people’s health and wellbeing and crucially health inequalities. We have seen throughout the pandemic individuals and the voluntary and community sector come together to provide magnificent support and help to individuals and families it is vital that we continue to focus local support on those most disadvantaged to help reduce the inevitable impact of this crisis.
I would once again, personally like to thank the people of Devon for how they have conducted themselves during the pandemic, adhering to the general public health guidance, testing guidance and isolation rules which has helped to keep infection rates as low as possible and help keep people safe.
I also wish again to offer my thanks to local service providers, partners, organisations and the community and voluntary sector who have continued their tremendous work, working together to respond to the needs of Devon residents during the pandemic.
It is important that people understand that COVID-19 is not over and achieving elimination is unviable, at least in the short-term. We all need to learn to live safely with covid for the foreseeable future. We are likely to see new variants which may well be more transmissible, and our current vaccines may offer less protection than against previous variants, so it is important that we all take responsibility to manage the covid risk to ourselves, our loved ones and to others in our communities. Our aim is to enable people to do this, and support those who cannot, so we can all live safely with covid.
Steven Brown
Director of Public Health
Recommendations
- Public Health Devon continues to maintain a surveillance system to monitor local cases and outbreaks across settings to enable swift public health actions, working closely with our partners.
- Public Health Devon continues to support NHS partners in the promotion and delivery of the COVID-19 vaccination programme, with a particular focus on addressing inequalities in uptake.
- Public Health Devon works with NHS partners to ensure the learning from the delivery of the COVID-19 vaccination programme is embedded in the delivery of all routine vaccination programmes.
- Further research should be commissioned to gain a greater understanding of food insecurity and fuel poverty in Devon, its impact and the arrangements to support people at greatest risk.
- Increase in publicity to raise awareness and encourage eligible homeowners in Devon to access free energy efficiency improvements through Cosy Devon.
- The Council continues to work with Government and local partners in the commissioning and delivery of schemes which mitigate some of the impacts of food and fuel insecurity, through funding within the Household Support Fund and Holiday Activities and Food programme.
- Public Health Devon work collaboratively with colleagues from Education and children and young people service providers to explore the delivery of an enhanced health and wellbeing programme offer.
- Local strategic partners should consider working together, with people with lived experience, to better understand the wider impacts of poverty and explore opportunities to help tackle and prevent poverty in Devon.
2. COVID-19 Update
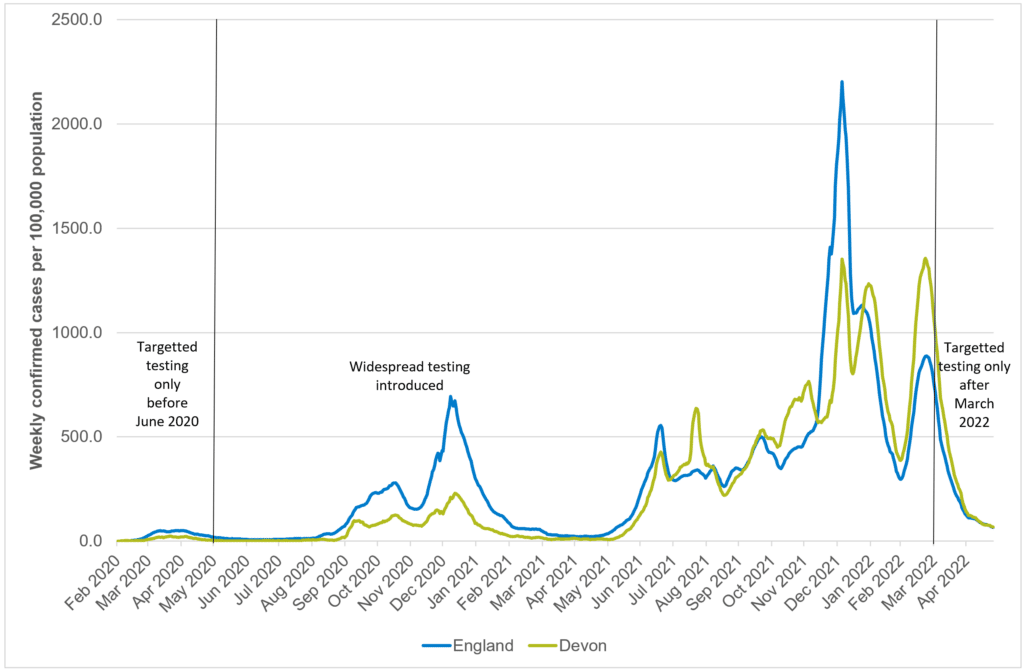
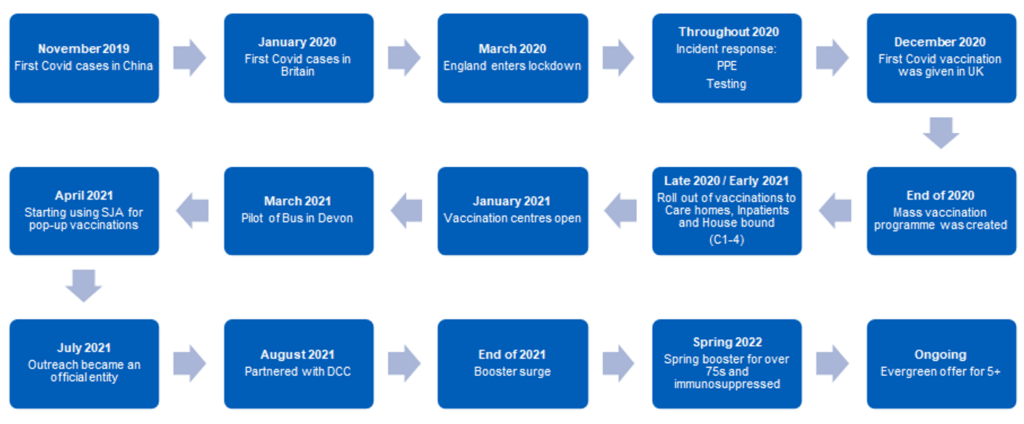
The COVID 19 pandemic continued through 2021/22. It is evident that restrictions such as the second and third lockdown in December 2020 and January 2021 and the rollout of phase 1 of the vaccination programme had an impact on case rates, hospitalisations and deaths during Spring 2021. Overall case rates, people admitted to hospital with COVID-19 and deaths during this period remained low and relatively unchanged.
Following the lifting of restrictions throughout Spring, by June 2021 there was a clear step change with case rates climbing to some of the highest rates for Devon over the course of the pandemic. There are many factors which may have influenced these increases. Restrictions over the course of this time were lifting and by the 19th of July, most legal limits on social contact were removed in England, and the remaining closed sectors of the economy were allowed to reopen. This coincided with the detection of the highly transmissible Delta variant which later became the dominant strain globally. Testing rates in Devon continued to be above the national average during this period and the number of people testing positive remained high following a pattern of multiple waves. Often increases in COVID-19 rates across younger age groups were a marker for anticipated increases across the general population. This was a typical pattern observed throughout the course of pandemic where increases in working age and older age population would follow the increases in cases in younger age groups. Despite higher case rates, hospitalisations and deaths remained lower during this time which was a clear indication of the efficacy and high uptake rates of the COVID-19 vaccine across Devon.
By the Autumn 2021, a new variant (Omicron) was detected. This particular variant spread more quickly than earlier variants. As such starker increases were observed both locally and nationally between Autumn 2021 and March 2022. This coincided with the cessation of the legal requirement to self-isolate at the end of February which would have also contributed to the higher COVID-19 rates during that time. In addition, given the staggered approach to the vaccine, waning of the vaccine started to become apparent and as well as higher case rates being observed, reinfection rates also increased. By March 2022, hospitalisations reached the highest peak observed throughout the pandemic in Devon and while deaths did increase over this period, this conversion rate was lower compared to the pre-vaccination phase of the pandemic.
Figure 2.1: Trend of COVID-19 case rates per 100,000 population across Devon
Source: UKHSA: https://coronavirus.data.gov.uk/
From the 1st of April 2022, free mass symptomatic and asymptomatic testing for the general public ended. This change in policy resulted in a significant drop in the testing rates with only a small number of people continuing to adhere to a regular testing regime, such as health and care front line workers and care home residents. The decline in overall testing resulted in a reduction in the number of people reporting a positive test result. While testing data reported a reduction in COVID-19 case rates, this was in reality much more to do with a reduction in the number of people testing rather than a true reflection of overall incidence both locally and nationally.
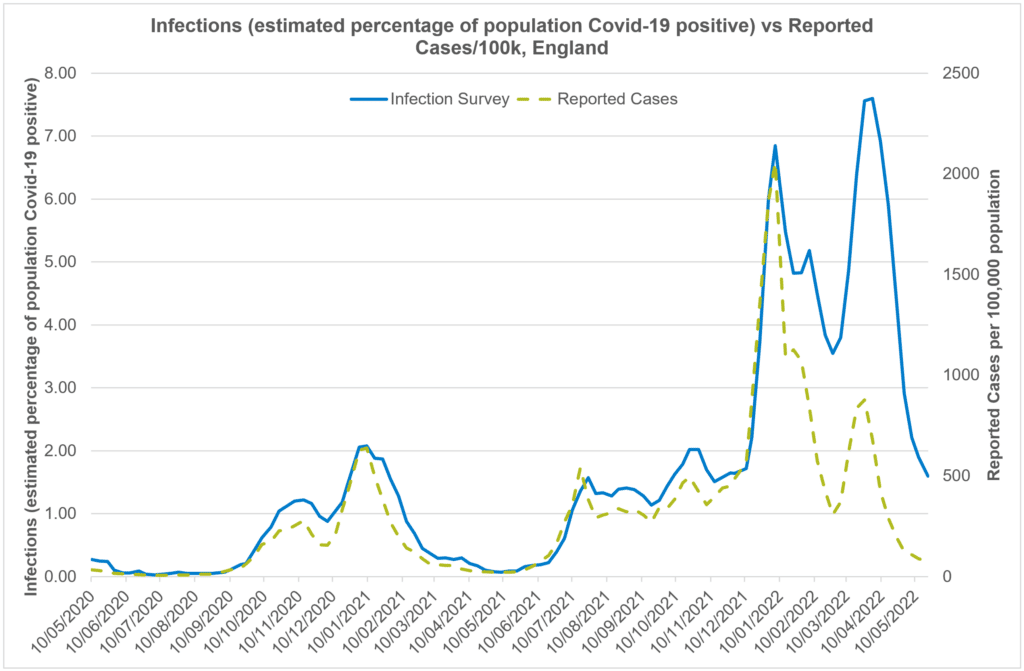
The Office for National Statistics (ONS) have continued to survey people and have been able to produce modelled estimates of COVID-19 incidence which has enabled us to monitor COVID-19 incidence rates (Figure 2.2). Overall, for the past few months, it is evident that an improving picture continues to be observed. The ONS estimates mirror a similar trend to the actual COVID-19 case rates indicating a continued reduction in COVID-19 incidence both locally and nationally. Moreover, hospitalisations and deaths continue to follow a similar trajectory. Good infection, prevention and control measures, vaccinations, and high antibody levels both have influenced an overall improving picture.
Figure 2.2: Trend of infections and reported cases per 100,000 population (England)
Source: Office for National Statistics Infection Survey Coronavirus (COVID-19) Infection Survey, UK Statistical bulletins – Office for National Statistics
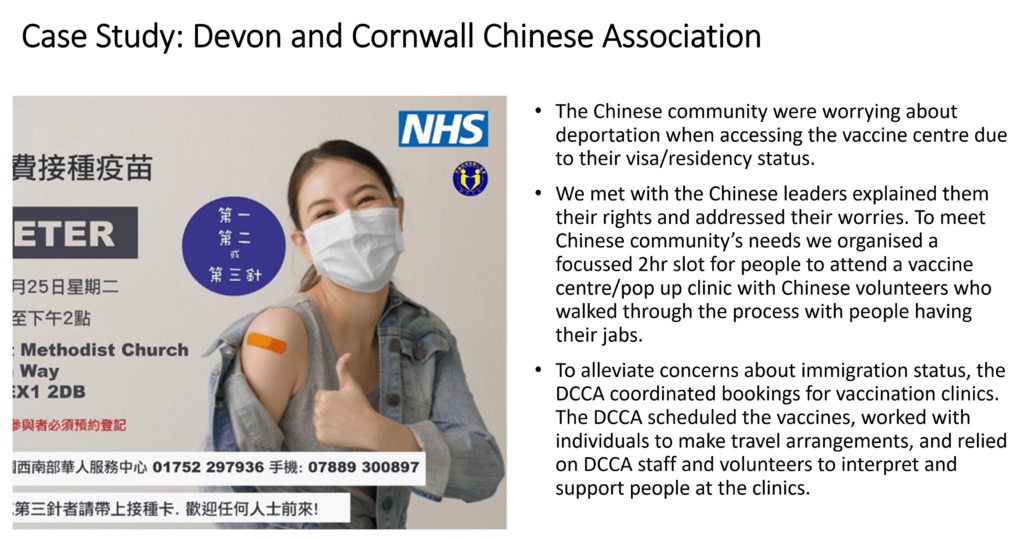
Vaccination has been our primary defence against illness, hospitalisation, and death. Devon has maintained a high level of uptake but not for everyone. In response, Devon was one of the first areas to launch a Health Inequalities Programme with greater focus on delivering vaccinations to different communities through an outreach vaccination approach, including use of mobile vaccination units and pop-up clinics in trusted community venues. By July 2021, Devon launched an extensive outreach vaccination programme. From May 2021 – 31st March 2022, 462 outreach clinics were held in Devon providing 49,297 vaccinations.
Figure 2.3 COVID-19 Vaccination timeline
The Pandemic has led to much richer intelligence on covid vaccination which has enabled us to take action at the local level. Variation in uptake is driven mostly by social and economic factors, with lower uptake in:
- younger age groups, especially males
- areas with higher levels of deprivation, especially younger age groups and clinically vulnerable groups
- non-White British ethnic groups – lowest in Black
- clinical risk groups compared to older age-specific cohorts
- people with severe mental illness
- people with learning disability
- people who are obese
- people who have Chronic Liver Disease
We have also worked closely with our partners and the community and voluntary sector to gather insight about barriers to uptake. An example of local intelligence and engagement leading to action to address inequality in uptake is outlined in the following case study.
Figure 2.4 COVID-19 Vaccination Case Study
It is difficult to predict with any certainty the future course of the pandemic but the Scientific Advisory Group for Emergencies (SAGE) have looked at a four possible scenarios from the worse case to best case scenario. The reasonable best case scenario indicates a comparatively small resurgence in infections during the coming autumn/winter and in the reasonable worst case scenario a very large wave of infection with increase levels of severe disease. As with all modelling during the course of the pandemic the likely answer is somewhere in the middle.
All the modelling undertaken by SAGE does indicate that we will reach a more stable position eventually but this will take several years. In the meantime we all have to learn to live with COVID-19. This means everyone taking some responsibility to do what they can to try and help keep rates as low as possible and importantly reduce the risk of transmission to those most vulnerable.
Reflection
It is important that people understand that COVID-19 is not over and achieving elimination is unviable, at least in the short-term. With the ceasing of mass testing, contract tracing and control measures such as the legal requirements to isolate if you test positive or the wearing facing covering in enclosed indoor areas our key defences against COVID-19 is the vaccination programme, encouraging behaviours through public health advice and ultimately managing covid as we would any respiratory illness.
The public health advice may have to change over time but the key advice remains the same If you are eligible for a vaccination please take up the offer as it will offer you the best protection against serious harm and if you have respiratory symptoms and are unwell stay at home if you can and try to avoid contact with other until you are feeling better.
Recommendations
- Public Health Devon continues to maintain a surveillance system to monitor local cases and outbreaks across settings to enable swift public health actions, working closely with our partners.
- Public Health Devon continues to support NHS partners in the promotion and delivery of the COVID-19 vaccination programme, with a particular focus on addressing inequalities in uptake.
- Public Health Devon works with NHS partners to ensure the learning from the delivery of the COVID-19 vaccination programme is embedded in the delivery of all routine vaccination programmes.
3. Wider Impacts of COVID-19 in Devon
3.1 Climate Change
Devon Strategic Plan Priority: Responding to the climate emergency
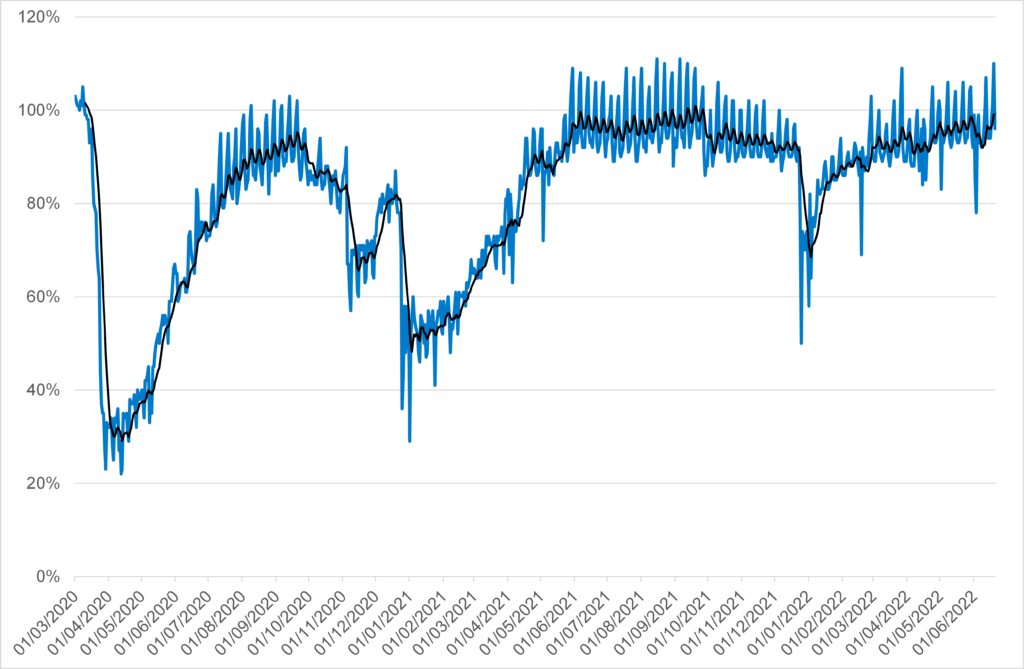
Climate change poses a serious threat to our quality of life, now and for future generations. It is damaging biodiversity, disrupting food production, damaging infrastructure, threatening jobs and harming human health. Addressing climate change requires a shift in our behaviour in relation to sustainable travel and reducing our carbon footprint in both our home and working lives. Whilst fundamental shifts in vehicle usage were observed during the pandemic, reflecting periods of lockdown where car usage fell by up to two thirds, as society has reopened car usage has returned to the pre-2020 baseline meaning some of the green benefits were short-lived.
Figure 3.1.1: Daily Car Usage in the UK as a percentage of baseline, 2020 to 2022
Source: Department for Transport, 2022 Transport use during the coronavirus (COVID-19) pandemic – GOV.UK (www.gov.uk)
In 2019 Devon County Council and other organisations in the county came together to form the Climate Emergency Response Group Devon Climate Emergency – Creating a resilient, net-zero carbon Devon – where people and nature thrive.. A Devon Carbon Plan and a Devon, Cornwall and Isles of Scilly Adaptation Plan are in development; and a wide range of projects have been launched.
The planetary and human health impacts of climate change were the subject of the 2019-20 Annual Public Health Report Devon Annual Public Health Report 2019-20 – Devon Health and Wellbeing. Air Pollution, excess heat and excess cold has a significant impact on our health, particularly in relation to increases in cases and deaths from respiratory and circulatory conditions like Asthma, Heart Disease and Stroke, with an increase in severe weather events leading to further direct risks to human health. For 2020, the Public Health Outcomes Framework estimated that 4.7% of deaths in Devon, and 5.6% of deaths in England were attributable to Air Pollution Public Health Outcomes Framework – Data – OHID (phe.org.uk).
3.2 The Cost-of-living Crisis
Devon Strategic Plan Priority: Tackle poverty and inequality
At the time of writing the report annual inflation is just over 9%, a 40 year high, with the Bank of England predicting inflation will peak above 11% before falling but fully expect price levels will remain high. Inflation is being driven by sharp increases in global energy and fuel prices, higher price of goods and domestic wage pressures. When inflation is driven by rising costs, as opposed to demand pressures, this form of inflation has a direct impact on living standards.
The Office for Budget Responsibility (OBR) projects that real disposable income will fall by 2.2% this year which would be the largest decline on record. This fall impacts those worst off most with low-income households and people living in poverty spending a larger share of their income on energy and food.
Increases in inflation not only has a direct impact on the health of the poorest households, described further in this chapter but also has an impact on people’s mental health. There is a strong correlation between deprivation and poor mental health. People with pre-existing conditions are likely to suffer most with an increased risk of stress and anxiety as they struggle with rising costs.
The COVID-19 pandemic has also contributed to the cost-of-living crisis in Devon. Since March 2020 demand for accommodation and the cost of housing have increased significantly. The economic and financial pressures seen through the pandemic, coupled with rising inflation and increasing energy, food and fuel costs mean that Devon citizens have been particularly affected.
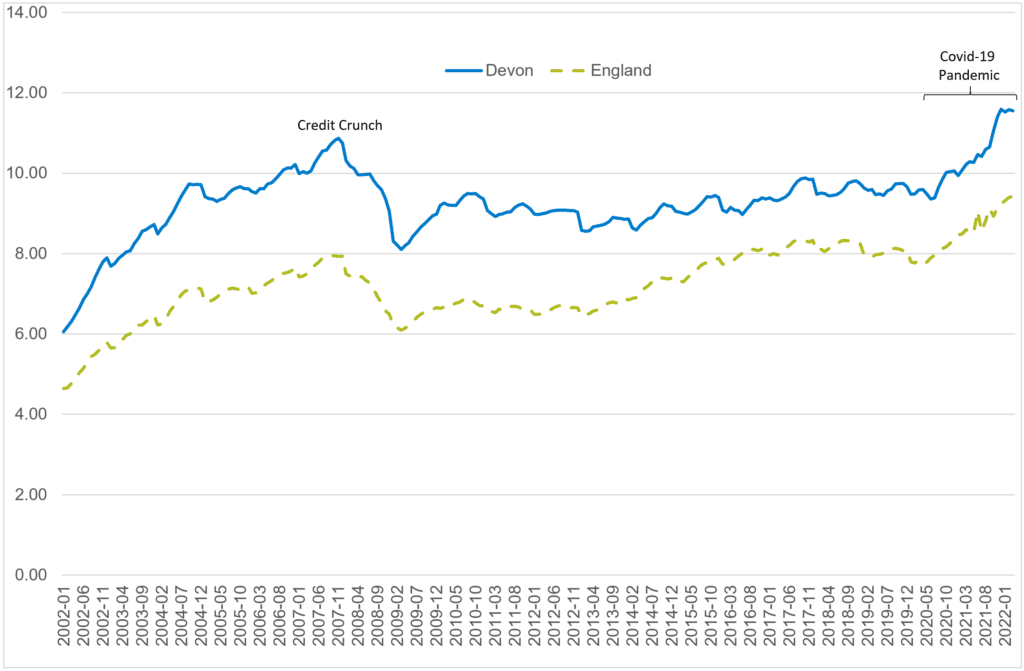
Whilst the cost of living is increasing across the UK, Devon is particularly vulnerable due to lower-than-average salaries, and above average housing and other costs. The COVID-19 pandemic contributed to increased housing costs and reduced financial security due to unemployment and the impact on local industries, including tourism and services. The demand for housing in Devon contributed to rising house prices, with the current average house price approaching 12 times higher than average annual full-time salaries in the County compared to just over nine times higher nationally, which rose sharply during the pandemic and are currently the highest on record.
Figure 3.2.1: Average House Price to Full-Time Salary Ratio, Devon vs England, 2002 to 2022
Source: Land Registry UK House Price Index (data.gov.uk) and Annual Survey of Hours and Earnings Nomis – Official Census and Labour Market Statistics (nomisweb.co.uk)
Average full-time salaries in Devon at £28,010 per annum are significantly lower than in England as a whole at £31,490 per annum, mean that Devon households are particularly vulnerable to increases in the cost of living. Key impacts include:
Food insecurity: research commissioned by the County Council in 2021 to establish the level of food insecurity in Devon found that approximately one in six (17%) of Devon households were experiencing food insecurity with one in ten households experiencing substantial disruptions to their eating patterns, with household members eating less and going hungry. Food prices grew by 6.7% in the year to April 2022 which some foods such as pasta increasing by 50%. Households living in poverty are least able to afford nutritious food and with rising prices this is likely to result in an unhealthy diet contributing further to poorer health outcomes. Responses to these households varies considerably across Devon’s geography and those most at risk of food insecurity can be the least likely to access available support. The Council’s delivery of Government funding such as the Household Support Fund has placed significant additional funding to local organisations and families.
Fuel/energy costs: UK households have seen a 54% increase in electricity costs this year and a 96% rise in gas costs. With the current price cap due to change in October 2022 it is predicted that prices will rise again. The current energy price cap is £1,971 with some commentators predicting the cap could rise to as much as £2,500-£3,000. Devon already has higher levels of fuel poverty (13%) than the UK (10%) and with the rising energy costs this is going to impact on a greater number of households in Devon. It is likely that households will be forced to make some very difficult decisions to put food on the table or heat their home, with the expectations that they will respond by cutting energy use. Living in cold homes has a direct impact on people’s health with an increase in cardiovascular and respiratory mortality associated with cold weather. The Council placed additional funding in 2020/21 to support energy support schemes for households via organisations including Citizens Advice.
Child Poverty: The proportion of children living in low-income families also reflects the impact of low wages, particularly in rural and coastal areas of the County. This is highlighted in the table below, which shows that the 10 wards with the highest proportions for this measure are in North Devon, Torridge and West Devon, rather than larger urban centres as seen historically.
Table 3.2.1: Percentage of children in low-income families, top 10 wards in Devon, 2021
| Ward | District | Children in Low Income Families (%) |
| Lynton & Lynmouth | North Devon | 27.2% |
| Chittlehampton | North Devon | 22.5% |
| Monkleigh & Putford | Torridge | 22.5% |
| Hartland | Torridge | 19.4% |
| Mortehoe | North Devon | 18.6% |
| Chulmleigh | North Devon | 18.4% |
| Drewsteignton | West Devon | 17.8% |
| Milton & Tamarside | Torridge | 17.5% |
| Hatherleigh | West Devon | 17.1% |
| Combe Martin | North Devon | 17.0% |
Source: Department of Work and Pensions Children in low income families: local area statistics – GOV.UK (www.gov.uk)
Access to health services: While the NHS is free at the point of delivery, many people pay for some of their healthcare. This can include for example prescription charges, opticians, dentistry, sexual health. As well as the service itself many people have travel costs associated with accessing health services. While those on the lowest income, are likely to have exemptions to some of the services above, the cost-of-living crisis is putting pressure on all households, and this may result in people deciding not to access health care which can have the impact of delaying diagnosis and treatment with may result in poor health outcomes.
3.3 Employment - how is the Devon economy bouncing back?
Devon Strategic Plan Priority: Support Sustainable Economic Recovery
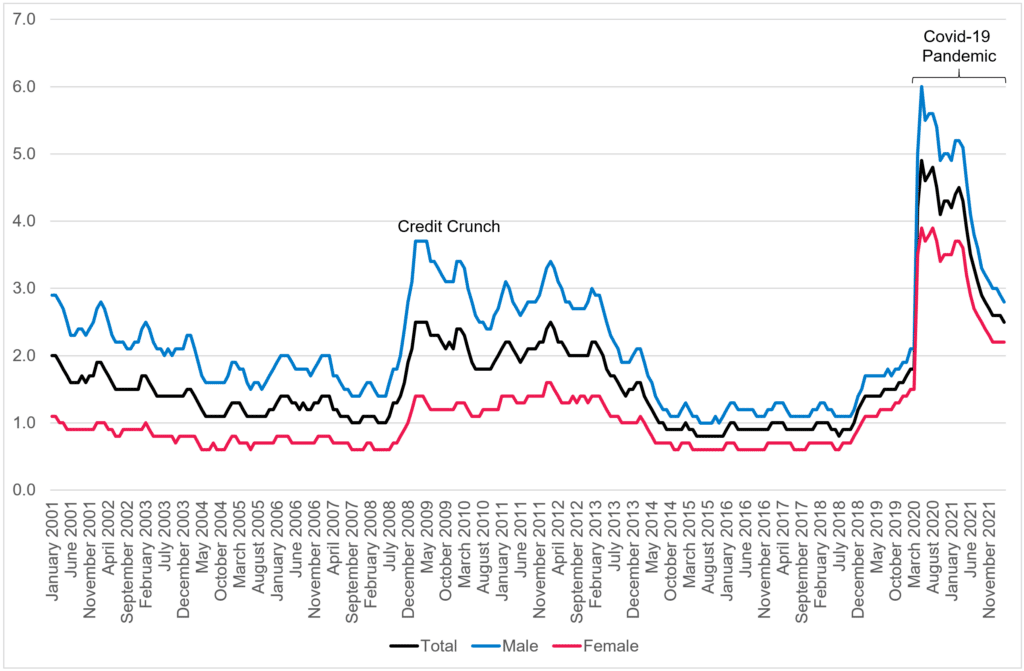
The COVID-19 pandemic led to a severe recession in 2020 with UK Gross Domestic Product falling by almost 10%. Whilst the economic recovery has been strong, challenges for the national and local economy persist. The cost-of-living crisis highlighted in a previous chapter has obviously significantly contributed to this.
Figure 3.3.1 shows trends in unemployment from 2001 to 2022 and highlights the severe impact that the pandemic had on the Devon economy, which was a much more severe economic shock than the credit crunch. Whilst economic recovery post pandemic continues, overall unemployment rates are still higher than during the credit crunch and subsequent recession, with unemployment levels amongst females particularly affected.
Figure 3.3.1: Jobseekers Allowance Claimants as percentage of working-age population, Devon, 2001 to 2022
Source: Department of Work and Pensions Claimant Count 2022 Nomis – Official Census and Labour Market Statistics (nomisweb.co.uk)
According to local economic assessment, other current economic issues in Devon include:
- Lower business confidence across the board due to rising cost base (energy, taxes, raw material inflation, wage inflation) and the potential for interest rate rises
- Ongoing labour shortages and the need to attract new workers and upskill existing ones. The existing exiting labour market is influenced by retirement, education and leaving UK
- Despite pay rises, real time wages in decline due to rising cost of living, which is widening income inequalities
- Business across the board face challenges during 2022/23 relating to cash flow, labour shortage constraints, limited investment and tax rises kicking in
- Growth ambitions remain in small and medium sized enterprises.
3.4 Long Covid: What has the impact been and who is most affected?
Devon Strategic Plan Priority: Improve Health and Wellbeing
‘Post-Covid syndrome’, known as ‘Long Covid’ for short, describes those experiencing longer term symptoms from a COVID-19 infection, lasting more than 12 weeks after their initial COVID-19 diagnosis and not explained by other conditions. Frequently reported symptoms include breathlessness, fatigue, confusion or ‘brain fog’, stress and anxiety. The effects can be debilitating and impact mental health and wellbeing. To address the effects of Long Covid, NHS England produced a five-point plan in October 2020, issuing clinical guidance, the ’Your Covid recovery’ platform to help people self-manage their recovery from Covid, and developed and funded local treatment services. As of April 2022, It was estimated that 1.3 million people in the UK (2.0% of the population) were still experiencing symptoms 12 weeks after contracting COVID-19 Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK – Office for National Statistics (ons.gov.uk)
Groups experiencing higher levels of Long Covid include:
- Those aged 35 to 69
- Females (rates are 41% higher than males)
- People living in more deprived areas (rates are 49% higher than less deprived areas)
- People employed in social care, health, teaching, retail and hospitality occupations
- People with existing health conditions (three times higher in the most clinically vulnerable compared to those with no health conditions)
It is currently estimated that around 16,000 people in Devon are still experiencing COVID-19 symptoms 12 weeks after contracting COVID-19. As with the national picture, those aged 35 to 69, females, people living in more deprived areas, people in care and close contact professions and those with long-term health conditions are at greater risk of developing Long Covid.
Around one in six (17%) of people estimated to be affected by Long Covid in Devon presented and were referred to Long Covid treatment services. Specifically:
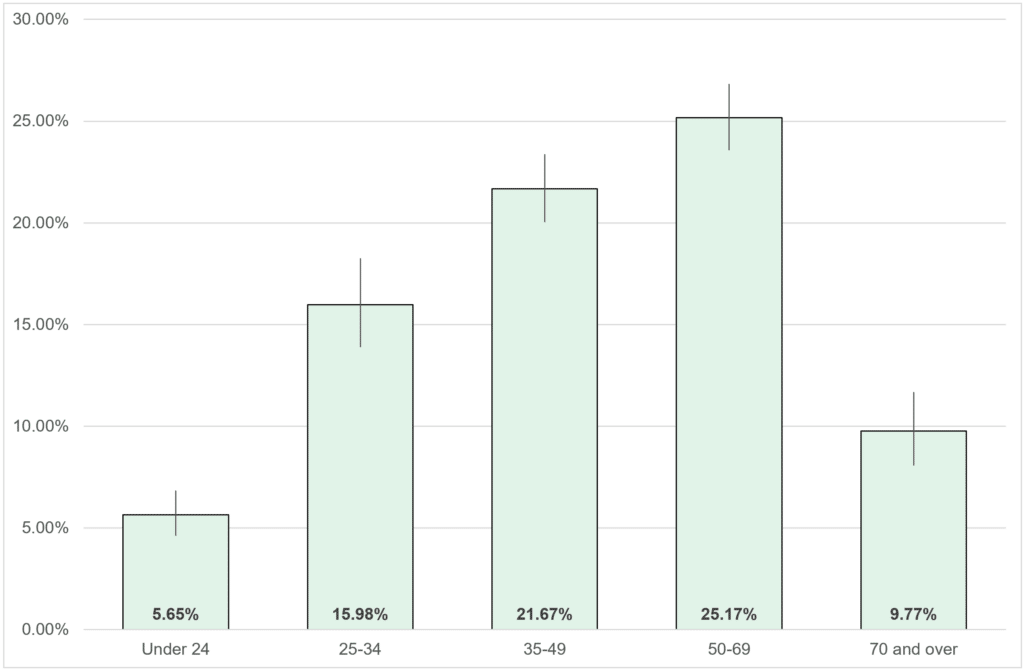
- Children and Older People were less likely seek help and be referred on to services (see figure 3.4.1 below)
- Men were less likely to seek help and be referred to services than females
- People living in more deprived areas were less likely to seek help and be referred.
Figure 3.4.1, percentage of those predicted to require long-covid service presenting and referred to services, Devon, 2021/22
Source: Devon County Council and Devon Clinical Commissioning Group, 2022
3.5 Mental Health
Devon Strategic Plan Priority: Improve Health and Wellbeing
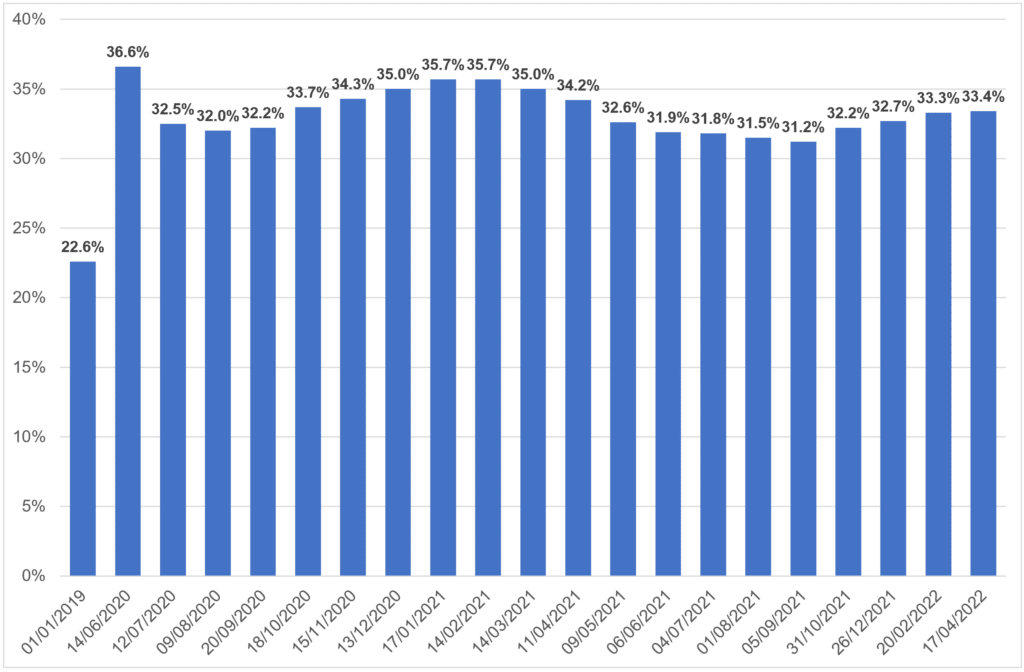
The Office for Health Inequalities and Disparities have produced a new set of reports focusing on the wider and longer-term impacts of the Covid-19 pandemic: Wider impacts of COVID-19 on health monitoring tool – GOV.UK (www.gov.uk). This includes a specific focus on mental health impacts, including the monthly tracking of mental health indicators. Increased mental illness, anxiety and loneliness; and decreased life satisfaction and happiness were seen throughout the pandemic and were particularly associated with periods of lockdown. Whilst these mental health impacts have been felt across the population, they have been more profoundly felt by people already experiencing greater disadvantage and health inequalities. As illustrated in figure 3.5.1 below, it is also evident that the initial improvements in wellbeing as society reopened in 2021, mental health indicators have worsened during early 2022, exacerbated by the cost-of-living crisis. Whilst this chart relates to adults, increased loneliness and mental ill health, and decreased wellbeing has been observed in both adults and children.
Figure 3.5.1: Adults with high anxiety score in Wellbeing Survey 2020-22 vs 2019 baseline, England
Source: Office for Health Improvement and Disparities 2022 COVID-19 mental health and wellbeing surveillance: report – GOV.UK (www.gov.uk)
3.6 Health and wellbeing pandemic impacts on children
Devon Strategic Plan Priority: Be ambitious for children and young people
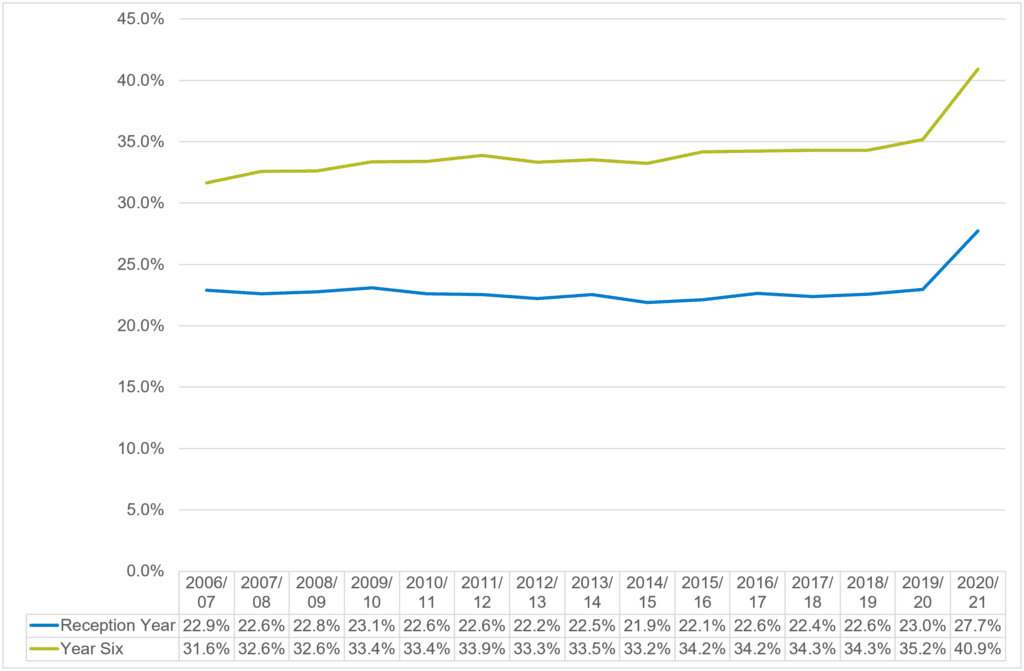
Increases in obesity in children and decreases in levels of physical activity have been observed in recent years nationally, exacerbated by the COVID-19 pandemic, Nationally the following patterns have been observed:
- An increase in obesity in reception year pupils (age 4 to 5) from 9.9% in 2019/20 to 14.4% in 2020/21
- An increase in obesity in year six pupils (age 10 to 11) from 21.0% in 2019/20 to 25.5% in 2020/21
- Higher levels of obesity in boys
- Children living in the most deprived areas are twice as likely to be obese than those in the least deprived areas
Figure 3.6.1 highlights how significant the increase in excess weight in children during 2020/21 was, with both reception and year six pupils experiencing the highest levels of excess weight ever recorded, which have been driven my lower levels of exercise and changes in diet and daily routines during the pandemic.
Figure 3.6.1: Excess Weight in Children by Year Group, England, 2006/07 to 2020/21
Source: NHS Digital 2022 National Child Measurement Programme, England 2020/21 School Year – NHS Digital
In terms of the health and wellbeing of young people in Devon a survey by the School Health Education Unit commissioned by Public Health revealed that in Autumn 2021:
- 7% of primary school pupils say they ‘never’ get a good night’s sleep, with 32% of pupils saying they only ‘sometimes’ do
- 47% of boys and 50% of girls worry about the environment; 46% of boys and 51% of girls about COVID-19; 32% boys and 35% girls about the future; 20% of boys and 24% girls about their weight or size; 30% of girls about the way they look
- 14% of primary school pupils said there has been violence between adults at home that frightened them
- 49% of year six pupils (aged 10-11) said they sometimes felt lonely and isolated during COVID-19, and 53% found it hard to focus on schoolwork
- 77% of year six pupils (aged 10-11) said their household had enough food for everyone everyday
- 29% of secondary school girls do not want to engage in physical activity because they are not comfortable in how they look, and 28% because they are shy in front of other people
- 21% of secondary school boys and 42% of secondary school girls have been picked on or bullied because of how they look; 19% of boys and 32% of girls have been picked on or bullied because of their size or weight
- 51% of year 10 girls (aged 14-15) think there is pressure on young people to have sex
- Amongst year 10 girls (aged 14-15), 15% had experienced a boyfriend / girlfriend telling them what to wear; 14% experienced hurtful or threatening language; 28% had a boyfriend / girlfriend who were angry or jealous when spending time with other people; 18% had a boyfriend / girlfriend who told them who they can and can’t see; 12% had experienced pressure to have sex or engage in sexual activity
- 33% of girls had been absent from school in the past 12 months because of their period (pain or access to sanitary products).
3.7 Community - how community organisations in Devon have supported since 2020
Devon Strategic Plan Priority: Help communities be safe, connected and resilient
Whilst the impacts of the pandemic have been considerable, community and voluntary sector organisations have played a vital role in supporting and strengthening communities
Local community and voluntary sector organisations were also supported through the Contain Outbreak Management Fund (COMF) to provide dedicate support in response to the impacts of COVID-19:
- Boosting citizens advice capacity to support COVID-19 recovery work
- Recruitment and awareness raising for existing and potential volunteers
- The development of the ‘Devon Connect’ platform and projects aimed at increasing digital inclusion
- A specific focus on reaching communities who are currently less engaged with services
- Community grants programmes to support small local initiatives
- Dedicated support to homeless, BME, LGBTQ+, and disabled people.
3.8 Reflections
The evidence presented clearly demonstrates the wider impact the pandemic has had on the health and wellbeing of Devon residents. Of particular concern is the rising levels of excess weight in children and the impact on people’s mental health. When you overlay the additional impact of the cost-of-living crisis, which like the pandemic is affecting everyone, but is disproportionality having the greatest impact on those worst off we are likely to see a worsening of health outcomes in the immediate future.
While recovery from the pandemic and the cost-of-living crisis is very much a global challenge we have demonstrated through the pandemic that local partners and communities can, and do, come together to support the most vulnerable living within their community. With a predicted rise in inflation, food prices continuing to rise and an increase in the energy cap, this winter is going to be very challenging for many families in Devon. Access to sufficient food and a warm home is going to be a priority.
Recommendations
- Further research should be commissioned to gain a greater understanding of food insecurity and fuel poverty in Devon, its impact and the arrangements to support people at greatest risk.
- Increase in publicity to raise awareness and encourage eligible homeowners in Devon to access free energy efficiency improvements through Cosy Devon.
- The Council continues to work with Government and local partners in the commissioning and delivery of schemes which mitigate some of the impacts of food and fuel insecurity, through funding within the Household Support Fund and Holiday Activities and Food programme.
- Public Health Devon work collaboratively with colleagues from Education and children and young people service providers to explore the delivery of an enhanced health and wellbeing programme offer.
4. Health Inequalities
Last year’s Annual Report focussed on the health inequalities that arose because of the Pandemic. As we learn to live with covid the impact of the pandemic continues, coupled with the cost-of-living crisis health inequalities will widen in Devon as the poorest households suffer the greatest impact.
We know that unemployment and poverty can cause both physical and mental ill-health, and further increase health inequalities, therefore the economic downturn linked to the pandemic will create new health challenges in Devon. It is increasingly important to build on and learn from some of the approaches developed through working so closely on a single issue with multiple impacts.
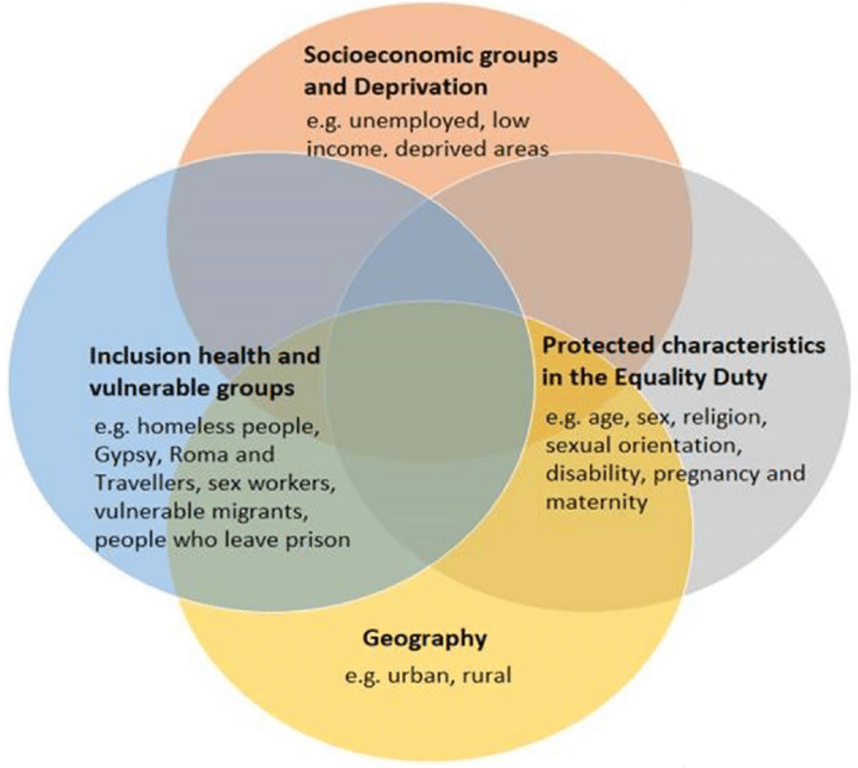
The Kings Fund (2020) describe Health Inequalities as ‘avoidable, unfair and systematic differences in health between different groups of people’. This applies to the status of people’s health but can also apply to the differences in the care people receive and opportunities they have to lead healthy lives, both of which can contribute to their health status. Health Inequalities can therefore involve differences in:
- health status, for example, life expectancy and prevalence of health conditions
- access to care, for example, availability of treatments
- quality and experience of care, for example, levels of patient satisfaction
- behavioural risks to health, for example, smoking rates
- wider determinants of health, for example, quality of housing.
The issues are not mutually exclusive, and individuals may be impacted by one or many of the dimensions described in the Health Equity Assessment Tool below. Health equity means ensuring that everyone has the opportunity to be as healthy as possible/optimal health.
Figure 4.1: Dimensions of Health Inequalities from the Health Equity Assessment Tool
Source: Health Equity Assessment Tool (HEAT): executive summary – GOV.UK (www.gov.uk) May 2021
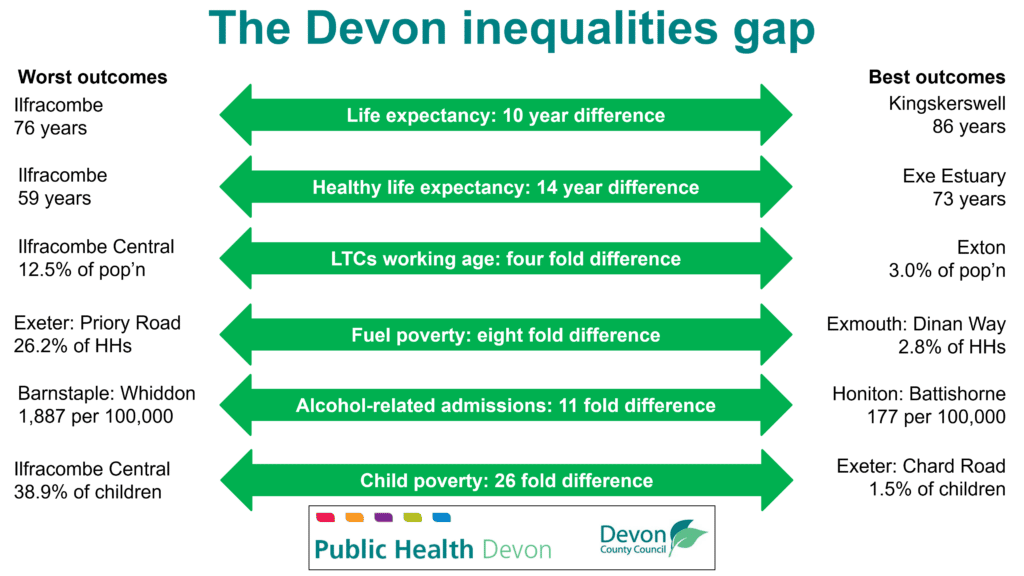
Tackling health inequalities is therefore a core part of improving access to services, the experience of services, and ultimately health outcomes for the whole population. Action on health inequalities requires improving the lives of those with the worst health outcomes, fastest. In Devon, for some there are significant differences due to the place a person lives.
Figure 4.2: Health Inequalities across Devon’s Communities
Devon is a sparsely populated County with many rural and coastal towns. The Chief Medical Officer’s annual report 2021: health in coastal communities – GOV.UK (www.gov.uk) states that there are many reasons for poor health outcomes in coastal communities. The pleasant environment attracts older, retired citizens to settle, who inevitably have more and increasing health problems. An oversupply of guest housing has led to Houses of Multiple Occupation which lead to concentrations of deprivation and ill health. The sea is a benefit but also a barrier: attracting NHS and social care staff to peripheral areas is harder, catchment areas for health services are artificially foreshortened and transport is often limited, in turn limiting job opportunities. Many coastal communities were created around a single industry such as previous versions of tourism, or fishing, or port work that have since moved on, meaning work can often be scarce or seasonal. Action to tackle health inequalities needs to reflect the context of where people live which are very different in different parts of the County.
In the Covid 19 Marmot Review: Build Back Fairer (2020) reducing health inequalities, including those exacerbated by the pandemic requires long-term policies with equity at the heart. Any local approach should consider equity of access, outcomes, and experience. The covid vaccination outreach programme is an example of where this can be applied in the short term whilst we seek to make long term lasting change and we are looking to apply the learning to other services and health interventions.
There are opportunities to make that change by working together with and for communities at a place-based level. Throughout the pandemic there are examples of how communities and those that work in them and for them could deliver support and services to meet local need. The approach resulted in continuous improvement through a focus on intelligence, insight, engagement and action. The engagement needs to build on best practice in effectively engaging with seldom heard groups and working with community champions.
The new Integrated Care System has health inequalities and mental health at its heart and is committed to making an impact as an Anchor Institution and through its delivery of services and partnership working. The NHS approach through Core20PLUS5 seeks to address inequalities in the most deprived areas with a focus on 5 clinical areas where health inequalities have a significant impact on health outcomes: NHS England » Core20PLUS5 – An approach to reducing health inequalities.
Devon County Council has a new Strategic Plan (2021-25) The best place – Strategic Plan (devon.gov.uk), and the priorities introduced in section 3 of this report have a strong focus on Health Inequalities and the importance of a good start in life through focusing on children and young people who have been so significantly impacted by the pandemic.
There has also been a focus on Inclusion Health throughout the pandemic. Inclusion Health is a ‘catch-all’ term used to describe people who are socially excluded, typically who experience multiple overlapping risk factors for poor health, experience stigma and discrimination, and are not consistently accounted for in electronic records. There is an opportunity to build on the Pandemic learning and make a lasting change and impact. We can learn from projects and programmes funded through the Contain Outbreak Management Fund. Assertive health outreach projects were funded in areas where homelessness and rough sleeping was high. Taking care to the individual improved access; addressed health needs and risk in relation to covid (thought vaccination and screening); but perhaps most importantly took a more holistic approach to addressing their health and wellbeing needs in collaboration with housing support, substance misuse and mental health services and the voluntary and community sector to support their broader needs.
Reflections
Professor Sir Michael Marmot in his report Health Equity in England (2020) identified that for the first time in 90 years life-expectancy has stopped increasing and health inequalities are widening. This research was published before the pandemic so we know the situation has worsened, poverty and inequalities have got worse. While central government has a key role in reducing health inequalities through national policy, locally we do have the ability to make a difference, impact on health inequalities and reduce poverty. The creation of the Devon Integrated Care Board (NHS Devon) and the Devon County Council Strategic Plan both identify tackling inequalities as a key priority. Local partners ensuring that due consideration is given to the impact on health inequalities for all their policy decisions is critical. Being able to answer the question, ‘in making this decision are we assured this this will help contribute to reducing rather than worsening health inequalities?’ Building this thought process into all out decisions will be critical to help tackle inequalities.
The report also highlights the excellent work which has taken place throughout the pandemic with communities, the voluntary sector and statutory partners coming together to provide support to vulnerable communities and families. It is vital that we build on and share this learning and there is ongoing commitment to continue to strengthen the relationships.
Recommendation
- Local strategic partners should consider working together, with people with lived experience, to better understand the wider impacts of poverty and explore opportunities to help tackle and prevent poverty in Devon.
5. Update on recommendations from 2020-21
| Recommendations 2020-21 | Update on Progress |
| Public Health Devon, working with colleagues within Devon County Council, the NHS and Public Health England, maintains a comprehensive COVID-19 surveillance system to provide real-time monitoring data to enable swift and decisive actions to any increase in cases or outbreaks | A public facing COVID-19 dashboard was developed and launched in August 2020. This dashboard describes the current levels COVID-19 cases, deaths within 28 days of a positive COVID-19 test and hospital beds occupied by persons with COVID-19 across Devon.
An internal COVID-19 Triangulation surveillance tool was developed in May 2020. This local tool provides real-time monitoring of tests, cases, hospitalisations, vaccinations and deaths data to inform swift decision-making to mitigate onward transmission of COVID-19 cases and manage outbreaks across a variety of settings in Devon. Public Health Devon launched and continues to maintain a Health Protection Response Hub to provide a rapid response to outbreaks and incidents across different settings, alongside the UK Health Security Agency. This has included the development of a comprehensive logging system to enable monitoring of situations. The hub is staffed by Health Protection and infection control specialists. |
| An effective local testing and contract tracing service, run by Public Health Devon, is maintained for as long as required to support the NHS Test and Trace service. | The Community Testing service started at three fixed sites and developed into an outreach programme with five mobile vans working with and within communities to increase access and support for testing with over a million tests delivered. The testing team expanded to include outreach vaccination building on the learning from testing.
The contact tracing service started small supporting the national service and at one point took cases immediately in identified postcode areas offering a local number and high response rate to ensure residents were supported to self- isolate. The contact tracing service worked closely with the Health Protection Response Hub to share early intelligence of cases and outbreaks in high-risk settings so that public health action could be taken. The testing and contract tracing service ceased operating following an instruction to do so by the DHSC at the end of March 2022. |
| The local authority’s health protection function is reviewed in the light of the pandemic and the relationship with the new UK Health Security Agency* (replacing Public Health England) is established. | Public Health Devon continues to work with the UK Health Security Agency (UKHSA) and regional and national health protection colleagues to manage the transition from post Pandemic working to Business as Usual. Funding has allowed this transition to be phased and we continue to run a Health Protection Response Hub to provide support to outbreaks and incidents alongside our UKHSA colleagues and NHS partners. |
| Lessons from reviews of the response informs how we prepare for and respond to future communicable disease outbreaks and shapes our recovery. | Throughout the pandemic there has been continuous learning which has required changes to be implemented swiftly to ensure we adapt to changing policy, demands and programmes. Whilst many debriefs have been undertaken, they also continue to ensure all learning is captured. |
| Devon County Council continues to work with NHS partners and other stakeholders to promote the uptake of the COVID-19 vaccination programme, with a particular focus on addressing inequalities in uptake. | Devon County Council has played a significant role in supporting delivery and uptake of the covid vaccination programme both through leading and championing work to drive uptake in the care sector and through leadership of a Health Inequalities Programme to increase uptake those most in need and seldom heard groups. The focus on health inequalities led to the establishment of a comprehensive and successful outreach vaccination programme, which has ensured that vaccinations have been offered in local communities, in trusted venues and to groups who may be least likely to access one of Devon’s mass vaccination sites. This work has since expanded to include a focus on both flu and covid vaccinations to ensure that our communities are fully protected this winter. |
| Public Health Devon continues to advocate for and contribute to Devon-wide, as well as place-based, plans for tackling poverty and reducing health inequalities | Public Health Devon continues to provide leadership and work with partners and stakeholders through the Devon County Council Strategic Plan, Climate Emergency response and Health Inequalities Programme of the Integrated Care System. |
| Public Health Intelligence Team and Smarter Devon, with stakeholders, coordinate the gathering and sharing of intelligence on the wider impacts of the pandemic in Devon and that this is used to inform partners’ recovery plans. | Smarter Devon and Public Health Devon have worked with Devon Communities Together to deliver a series of interactive workshops to determine the impacts of the pandemic on the people of Devon. This culminated in a report (September 21) and a Power BI Dashboard that brings together relevant datasets to highlight those areas of need across Devon. The Dashboard will be received by Team Devon in July 2022 and this will ensure future plans for the recovery will be based on evidence. |
| Public Health Devon continues to advocate for a collaborative, cross-sector asset-based approach to reducing inequalities ensuring that communities’ assets, priorities and perspectives are understood by, and inform the support offered by, organisations. | Building on the learning from working with communities throughout the Pandemic Public Health Devon seeks to listen to the voices and experiences of those with the worst health outcomes and access to inform support offers.
To support this recommendation, Public Health Devon commissioned a sample survey of Devon residents to understand the extent and experience of food poverty in Devon. The results of the survey have been widely publicised and are helping us to make the case for additional support for families struggling in Devon. |
| Recovery programmes should be based on the evidence of what works to reduce health inequalities. | The Devon Recovery Co-ordinating Group have been using intelligence and insight alongside the evidence base (where it exists) to inform decisions and action. For example, the Devon Food Partnership development work. The South West Recovery action cards produced by the Office for Health Improvement and Disparities (OHID) provide a useful reference point for this purpose. |
| Review how agencies’ policies and programmes and the use of impact assessment tools harness the potential we have for addressing the climate emergency and reducing inequalities | Public Health Devon have been working with the Organisational Change Team and Smarter Devon to trial a new tool that will help us assess the Social and Environmental impacts of our decisions. This tool is based on the Doughnut Economics concept developed by Kate Raworth. |
6. Summary of Joint Strategic Needs Assessment (JSNA)
Introduction
Devon has an ageing and growing population, with proportionately more older people compared to the population structure of England. The growth in the Devon population is attributable to longer life expectancy, internal migration and increases in planned development.
In Devon there are many population groups across the life course that experience inequalities in health and wellbeing outcomes. This blend of different population groups presents opportunities in how we as a system support the varying needs of the Devon population.
Health and wellbeing outcomes follow a social gradient which shows us that as deprivation increases, the risk of poorer outcomes increases. There is a notable north-south division which much of East Devon, South Hams and Teignbridge being less deprived compared to North Devon, Torridge and West Devon.
A focus on an upstream approach to improve population health and wellbeing is required to prevent ill health and enable those to live healthier for longer, for early detection of disease and treatment, and to and maintain a good quality in life in those with a long-term condition.
Poorer mental health has a great social and economic impact. It can affect people at any stage of the life course and can diminish the life chances of individuals significantly impacting physical health, educational and employment prospects, and life expectancy. Equally, poor physical health can lead to an increased risk of developing mental health problems. Just with physical health, inequalities can be found in mental health. This gap is even great for those with severe mental illness.
Important: Disparities in health and wellbeing outcomes are even starker when looking across smaller areas and/or different population groups across Devon.
Starting and Developing Well
Across Devon there are proportionately fewer younger people when comparing nationally. Health and wellbeing outcomes for children and young people across Devon is mixed.
There are considerable opportunities and benefits in improving interventions to support best start in life which include reducing smoking during pregnancy, increasing new birth visits, sustaining and improving breastfeeding from 6 to 8 weeks, improving health protection measures such as handwashing and increasing immunisation coverage particularly for children in care.
A focus on improving behavioural risk factors for children and young people around diet and physical activity is required to reduce dental decay in younger children and obesity in primary school aged children.
Whilst a fair proportion of children at the end of reception reach a good level of development, around a quarter of pupils are not achieving this level which may have an impact throughout their life. This gap in school readiness is considerably wider for disadvantaged children.
Poor mental health in children results in poorer outcomes relating to health and wellbeing. Hospital admissions in children and young people are considerably higher in Devon for mental health conditions, self-harm and injuries. This gap is even wider for vulnerable groups such as disadvantaged and looked after children. In addition, some children and young people’s mental health and wellbeing has been substantially impacted during the pandemic.
Living and Working Well
Devon has proportionately fewer working age people compared to England, particularly in those aged 16 to 49 years. Despite some reductions observed throughout the pandemic in economic activity, economic activity in Devon remains higher than the England average. However, the sectoral composition across Devon creates low earnings employment. This impacts on a variety of wider determinant factors which influences health and wellbeing. The COVID-19 pandemic has significantly impacted upon the economy and the cost of living which will increase poverty and health inequalities.
Life expectancy has remained marginally similar over the last decade with people living their remaining 10 to 15 years of life in poorer health. This gap is starker across areas with higher deprivation, and particular groups and communities. Whilst improvements have been ascertained across some behaviour risk factors and, better treatments and technological advances have contributed to better health and longer life expectancy in general, more work is required to improve diet, physical activity, alcohol intake and smoking. These are the leading behavioural risk factors which influence ill health and preventable mortality across Devon. Obesity in particular is increasing worldwide and the associated factors which influence obesity include deprivation, socio economic issues, poor diet and lack of physical activity have also been impacted by the COVID-19 pandemic. Therefore, it is expected that increases in obesity levels will be observed both locally and nationally as a result.
Poorer health can further manifest downstream. It can impact on the ability to work which may lead to receipt of state benefits and/or creating more cost across the health and social care system for treatment and support-based services. If the population of Devon are living between 10 to 15 years in poorer health and require treatment and support, evidently it will be significant and increasing cost to the system.
There are opportunities to improve primary and secondary prevention such as increasing immunisation and screening coverage and improving health protection measures to prevent ill health, reduce disease progression and mortality from many diseases.
Ageing and Dying Well
Devon has an ageing and growing population with proportionately more older people compared to England. As identified in the ‘Living and Working Well’ section, life expectancy has marginally changed over the last decade, similar to mortality rates from conditions considered preventable. Furthermore, people across Devon are living on average between 10 and 15 of their final years in poorer health which will have a significant impact on service cost and demand across the system.
Devon is generally less deprived overall relative to England, however disparities relating to how deprived or how affluent areas across Devon do exist which can influence health and wellbeing outcomes. Devon boasts a beautiful landscape with a third of the county classified as rural. However, this presents challenges around access to services and isolation contributing to poorer health outcomes.
The development of frailty, long term conditions and multi-morbidity is impacted greatly by social and behavioural risk factors. This can be influenced by poorer mental health or poor physical health may lead to poor mental health. This impact is even greater where inequalities are a considerable challenge.
Cancer, diseases of circulatory, respiratory, nervous system, and mental health and behavioural disorders are the leading causes of death across Devon. From a seasonal perspective, higher excess winter deaths occur in older people with pre – existing circulatory and respiratory diseases. Across Devon excess winter deaths have remained relatively unchanged. However increased uptake of primary and secondary interventions such as immunisations and screening programmes may help to reduce excess winter deaths. Across the UK the COVID-19 pandemic has impacted upon planned and attended appointments both in primary and secondary care particularly during the first and second lockdown. Delays on waiting lists, cancellations of referrals and procedures, lack of staffing capacity and health seeking hesitancy due to COVID-19 may contribute to delayed diagnosis and poorer outcomes in the future.
Immunisations for flu in those aged 65 and over, and at-risk individuals, and PPV are all below the recommended targets for uptake. Whilst uptake for flu immunisations aged 65 and over is improving, flu immunisation for at risk individuals and PPV immunisation has not significantly changed for a number of years. COVID-19 vaccinations overall across Devon remain high, however uptake is lower across certain age and minority groups. Cancer screening for bowel, cervical and breast indicate that uptake for Devon is higher compared to national uptake rates. However, around 1 in 4 people within those target groups are not being screened.
Dementia diagnosis remains unchanged in Devon and highlights a potential gap of unmet need where 2 in 5 people aged 65 and over are estimated to have dementia but are undiagnosed.
From an inequalities perspective immunisations and screening, and incidence and mortality rates may also differ when looking at more deprived areas and cohorts with protective characteristics. Therefore, in some instances the gap in outcomes may be wider.
To conclude, the Devon population is diverse in its needs and inequality can take many forms which impacts population health, to which organisations from across the system need to respond.
7. Acknowledgements and Further Information
If you would like this report in a different format, such as large print or Braille, please contact:
Public Health Devon, County Hall, Topsham Road, Exeter, EX2 4QD
Phone: 01392 383000
Email: publichealth@devon.gov.uk
This annual report has been written by Steven Brown with input from Sara Gibbs, Tina Henry, Simon Chant, Maria Moloney-Lucey, Sarah Ogilvie, Charlotte Pavitt and Rebecca Shuttleworth.
Published by Devon County Council 2022
Copyright Devon County Council 2022